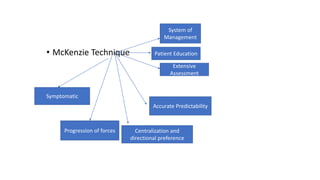
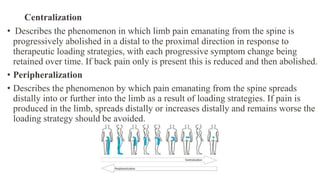
The McKenzie method is a mechanical-based classification and treatment approach for musculoskeletal disorders introduced by Robin McKenzie in 1981. It involves assessing a patient's symptoms in response to standardized movements to classify them into mechanical syndromes. The goal is to identify a directional preference that centralizes or reduces pain through repeated end-range movements. Exercises are then prescribed matching the patient's directional preference to improve symptoms and restore full function. The McKenzie method aims to involve patients through education and self-management of their condition.