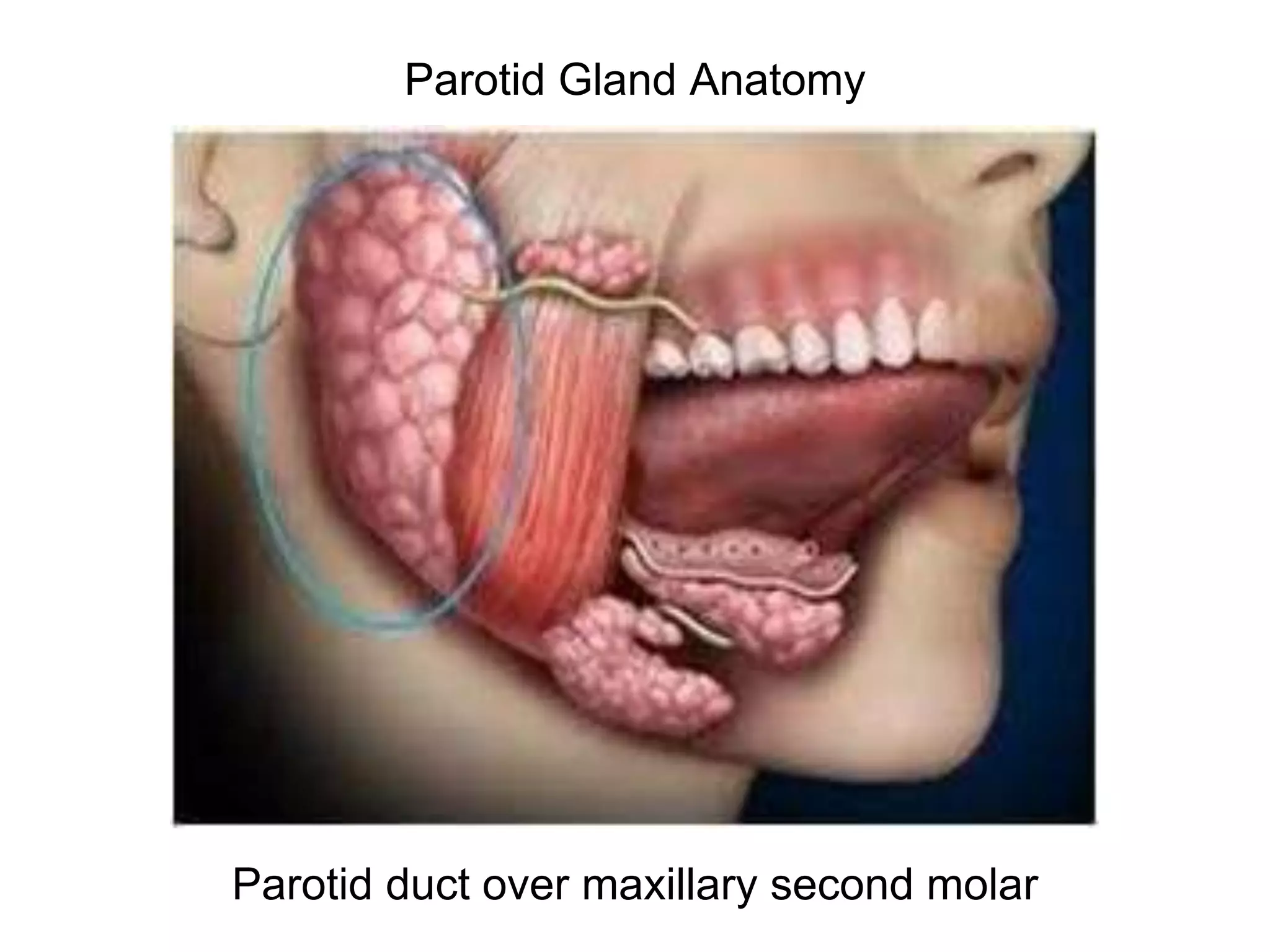
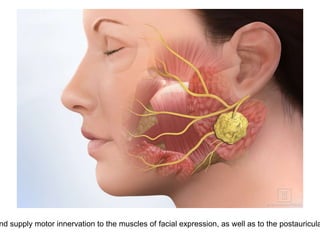
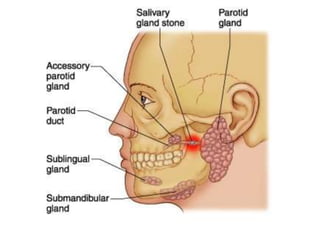
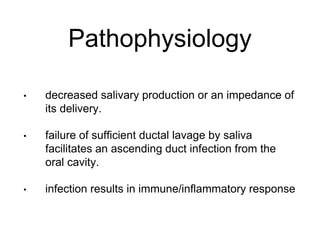
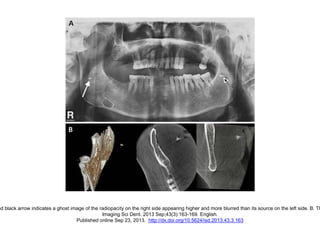
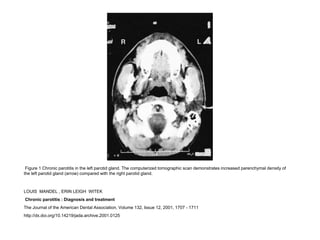
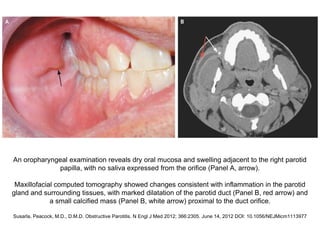
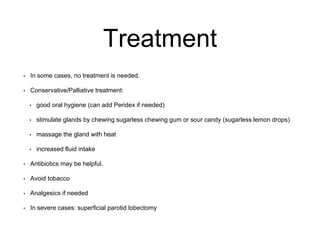
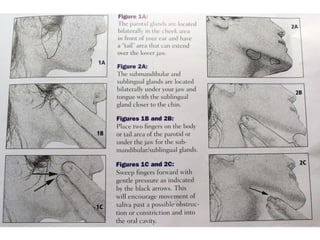
Parotid gland anatomy and pathophysiology of parotitis are described. Parotitis is inflammation of the parotid gland most commonly caused by viral or bacterial infection when saliva production is decreased. Symptoms include pain, swelling, and pus draining from the parotid duct. Diagnosis involves medical history, physical exam, and imaging tests. Treatment ranges from conservative measures like antibiotics, heat therapy and increased fluids to surgery in severe cases. Complications are rare if treated properly.