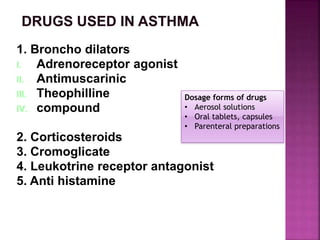
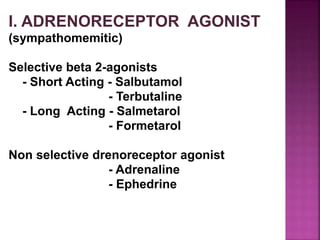
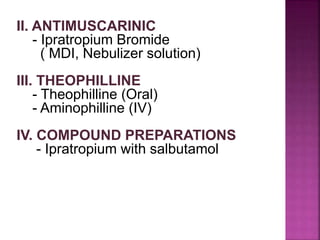
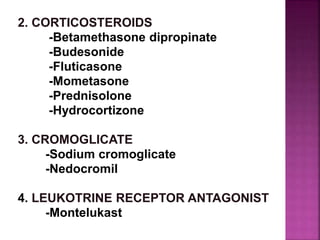
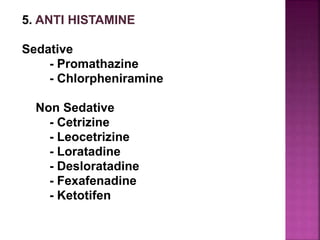
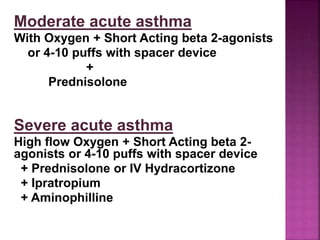
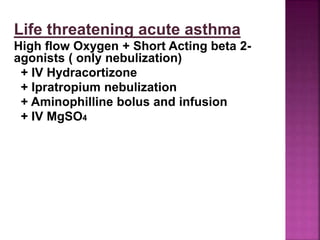
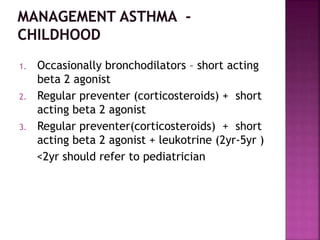
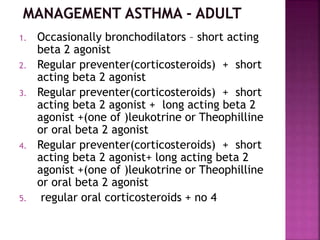
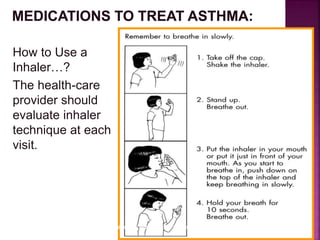
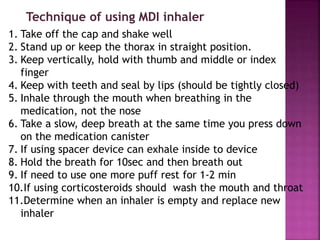
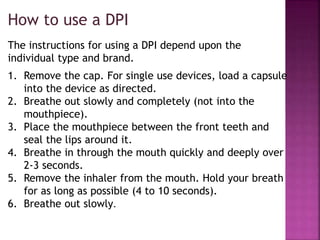
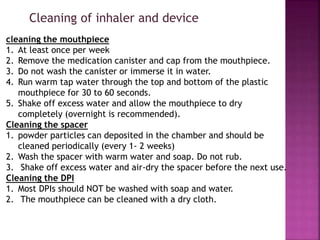
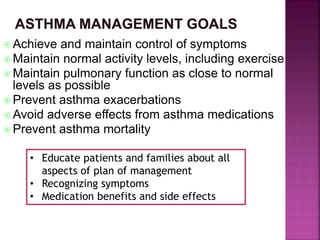
This document discusses asthma, including its symptoms, diagnosis, treatment, and management. It defines asthma and an asthma exacerbation. It outlines the medical history and symptoms to assess in a patient. It describes lung function testing, classifications of asthma severity, and long-term control versus quick relief medications. It provides details on common asthma medications and inhaler devices. It offers guidance on treating mild, moderate, and severe asthma exacerbations. It discusses developing an asthma action plan and the goals of treatment and management.