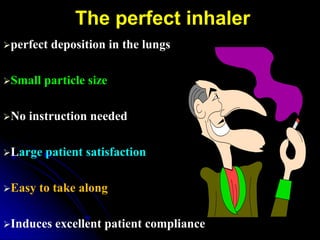
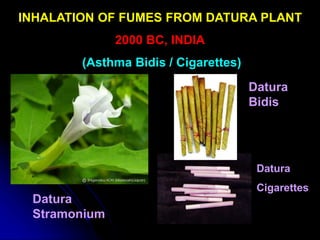
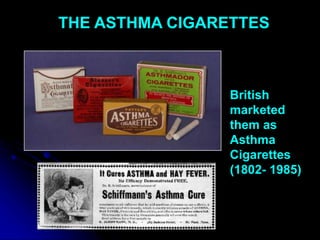
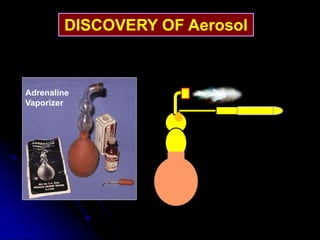
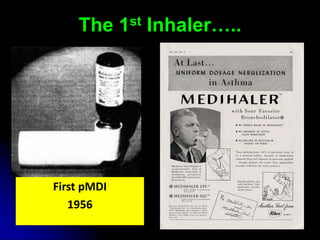
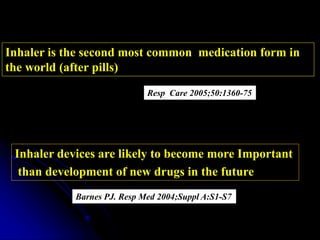
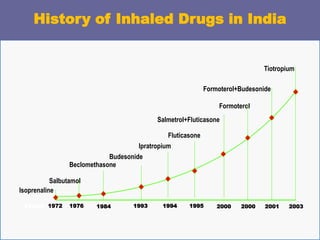
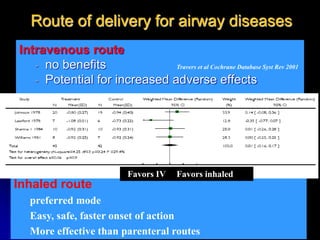
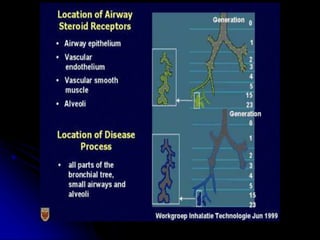
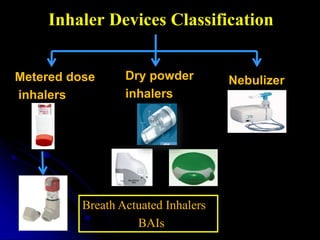
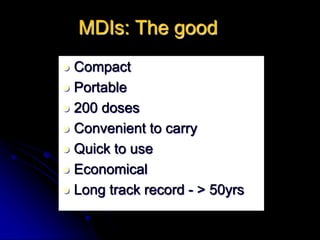
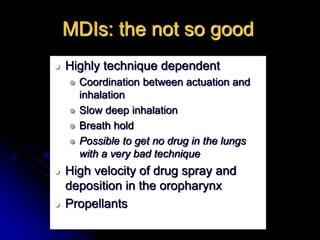
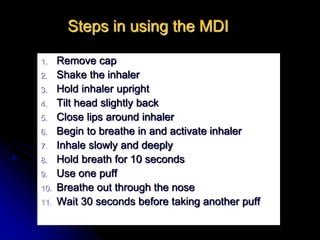
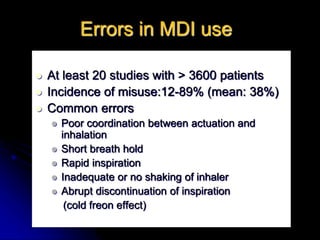
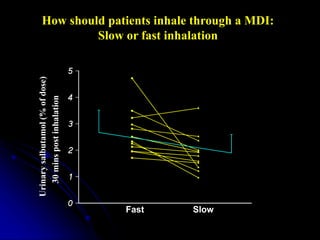
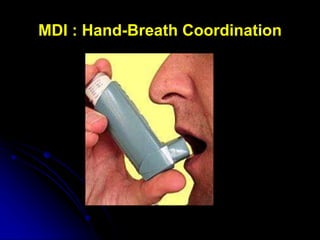
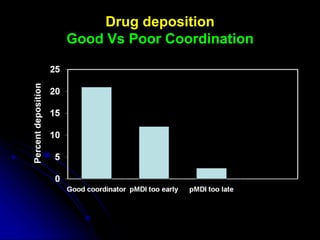
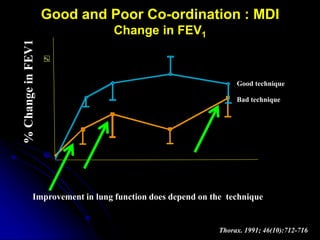
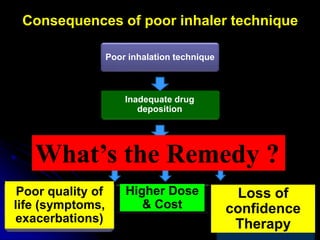
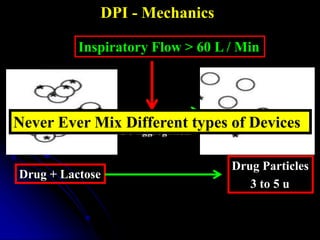
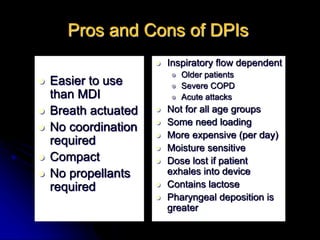
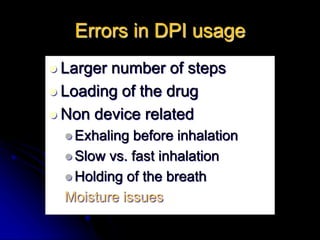
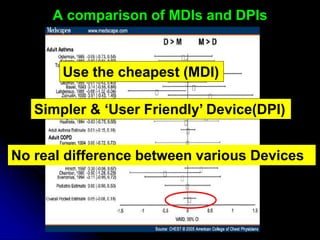
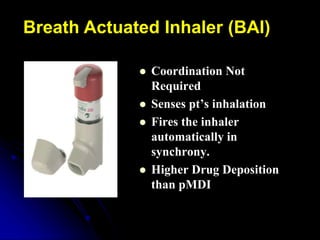
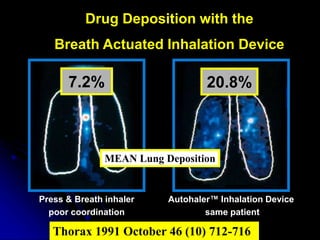
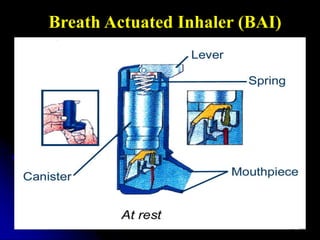
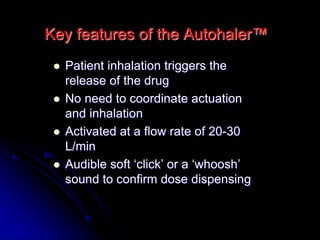
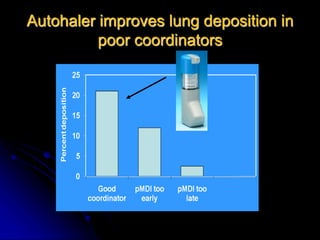
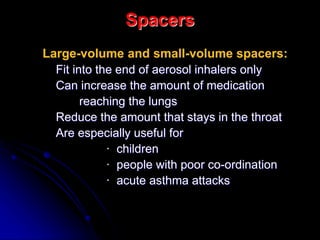
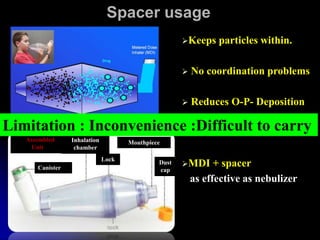
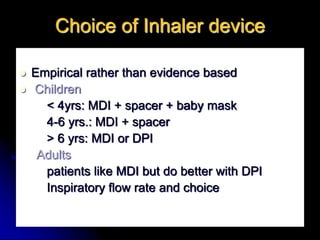
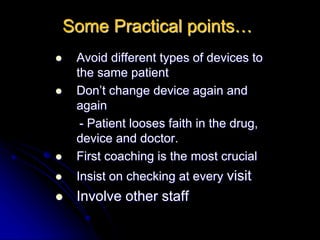
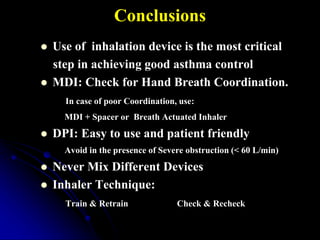
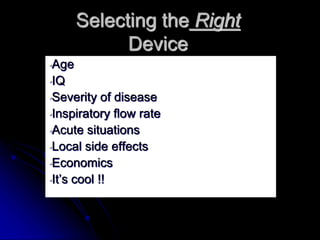
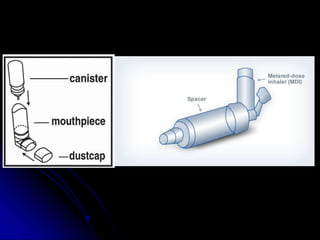
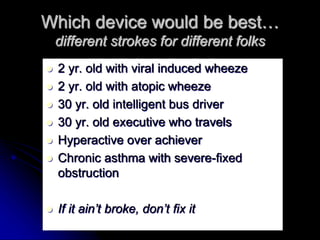
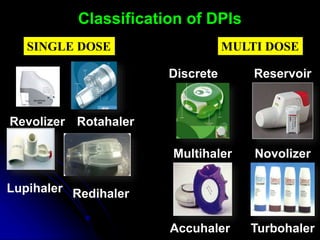
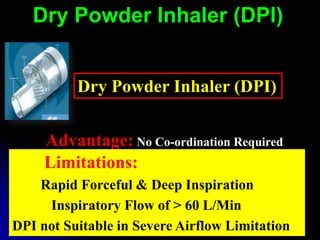
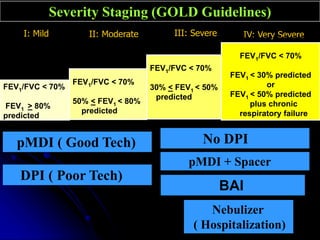
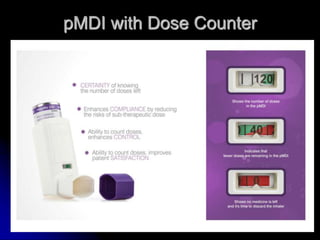
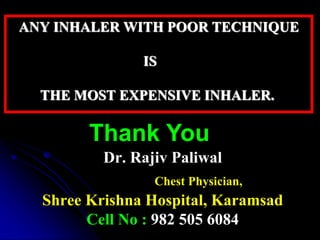
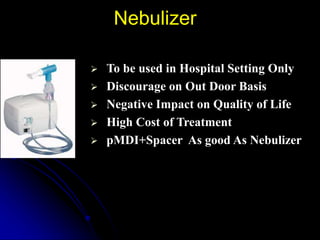
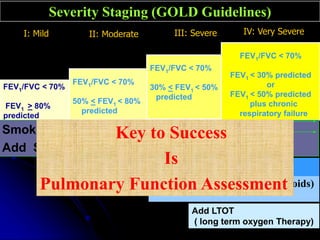
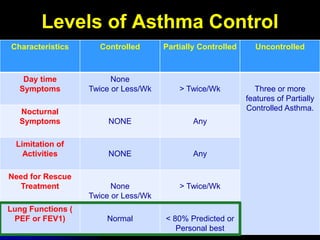
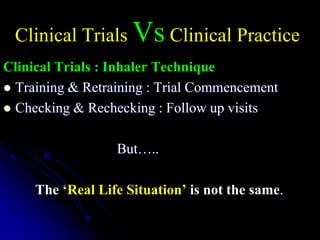
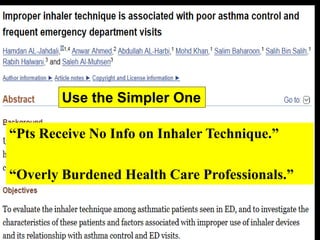
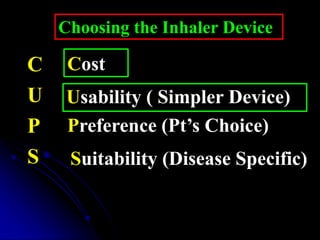
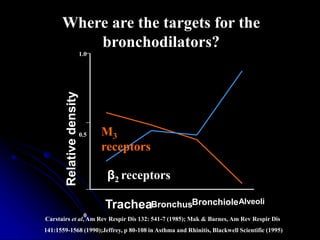
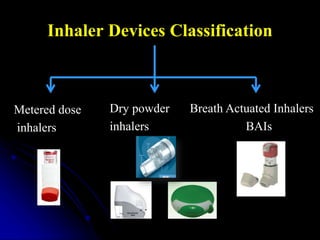
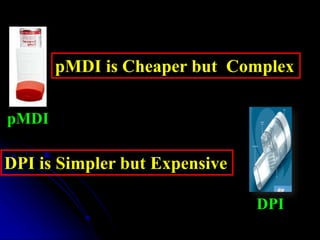
The document discusses inhaler devices for asthma control. It provides a history of inhaler devices from ancient times to modern devices. It describes different types of inhaler devices including metered dose inhalers, dry powder inhalers, nebulizers, and breath actuated inhalers. It discusses factors to consider when selecting a device including a patient's age, inspiratory flow rate, severity of asthma, and acute situations. The document emphasizes the importance of inhaler technique and ongoing training to ensure proper use.