The document discusses congenital malformations, including:
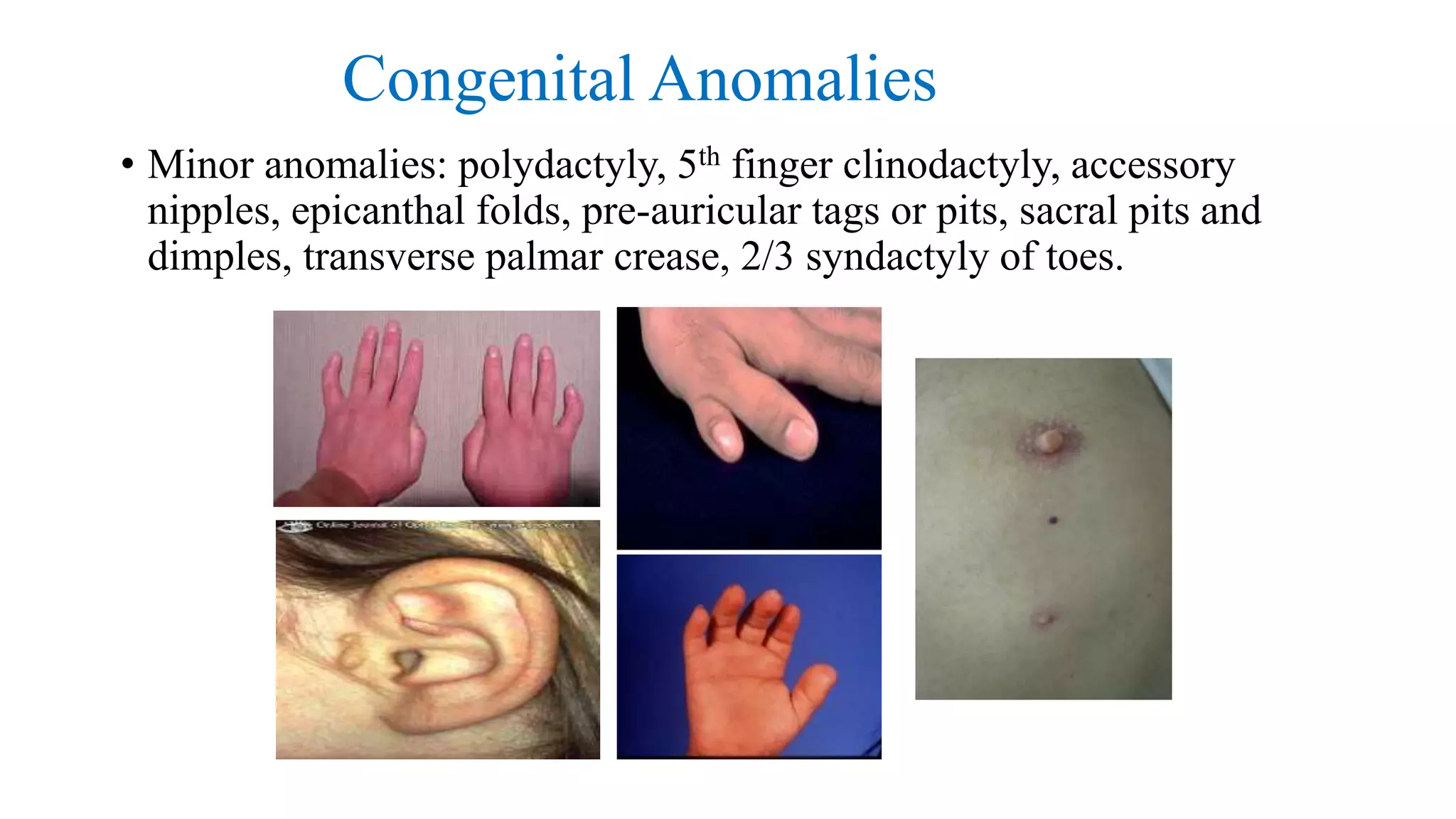
- Types of congenital anomalies like major anomalies that interfere with normal functioning and minor anomalies that have only cosmetic significance.
- Causes of congenital anomalies which can be genetic like chromosomal or single gene defects, or non-genetic like drugs, infections, or maternal illness.
- Stages of normal morphogenesis and how abnormalities can occur if stages are incomplete, take an aberrant form, or functional defects develop. Timing of different malformations is outlined.
- Specific genetic syndromes are mentioned as causes for different malformation patterns. Deletion 22q11 syndrome is discussed in detail as a common microdeletion syndrome.