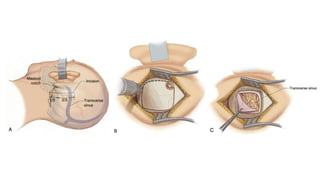
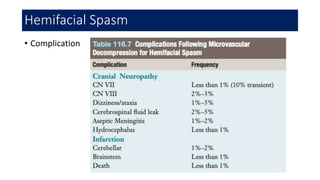
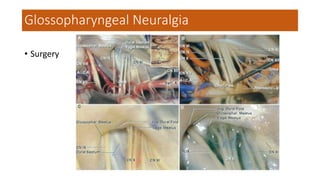
Microvascular Decompression is a surgical procedure used to treat trigeminal neuralgia, hemifacial spasm, and glossopharyngeal neuralgia caused by compression of cranial nerves by blood vessels. The procedure involves using a microscope to identify the compressing blood vessel and place a small piece of Teflon between the nerve and vessel to relieve compression. It provides long-term pain relief with few complications when performed by an experienced surgeon for patients who have not responded well to medications.