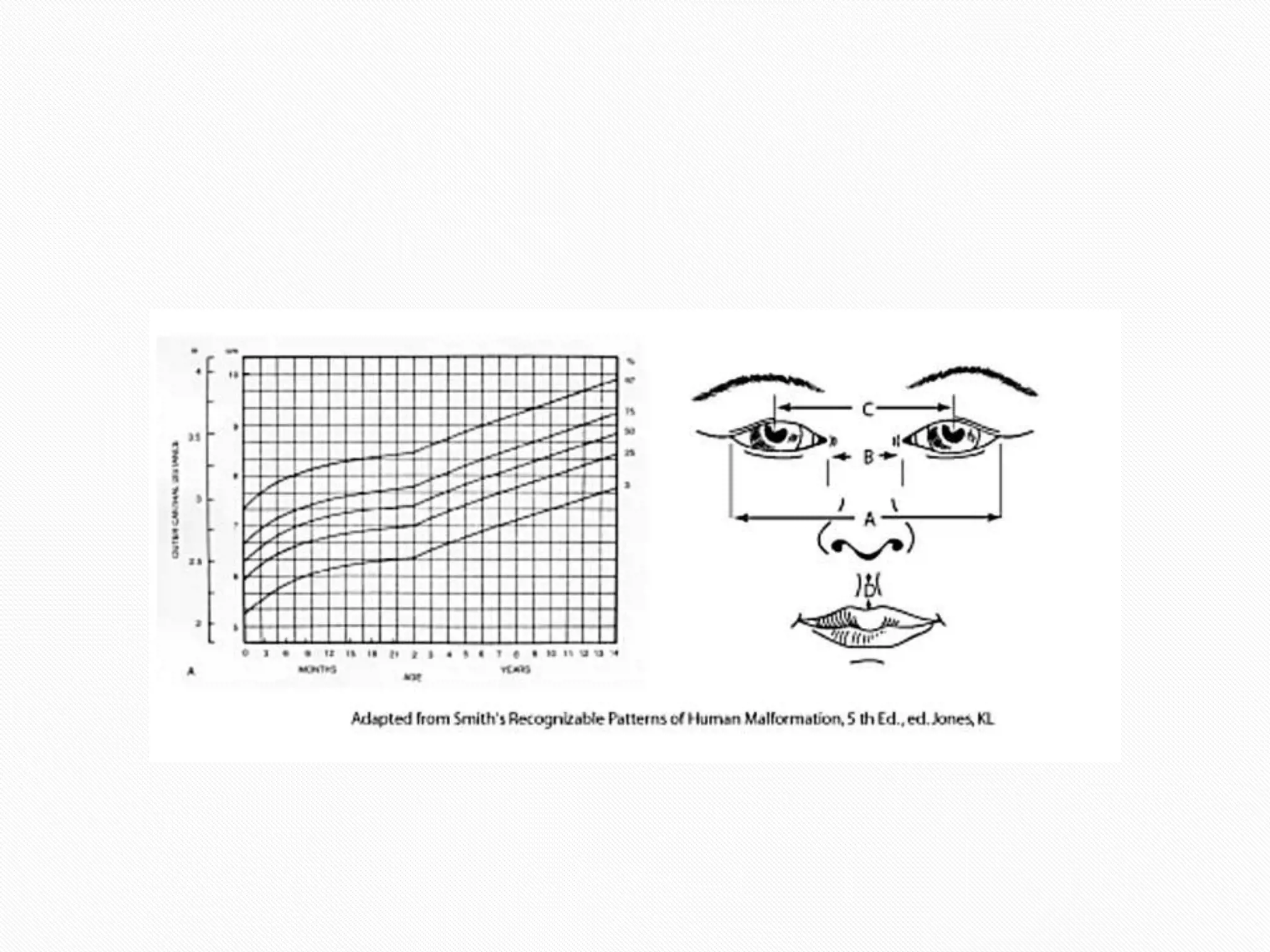
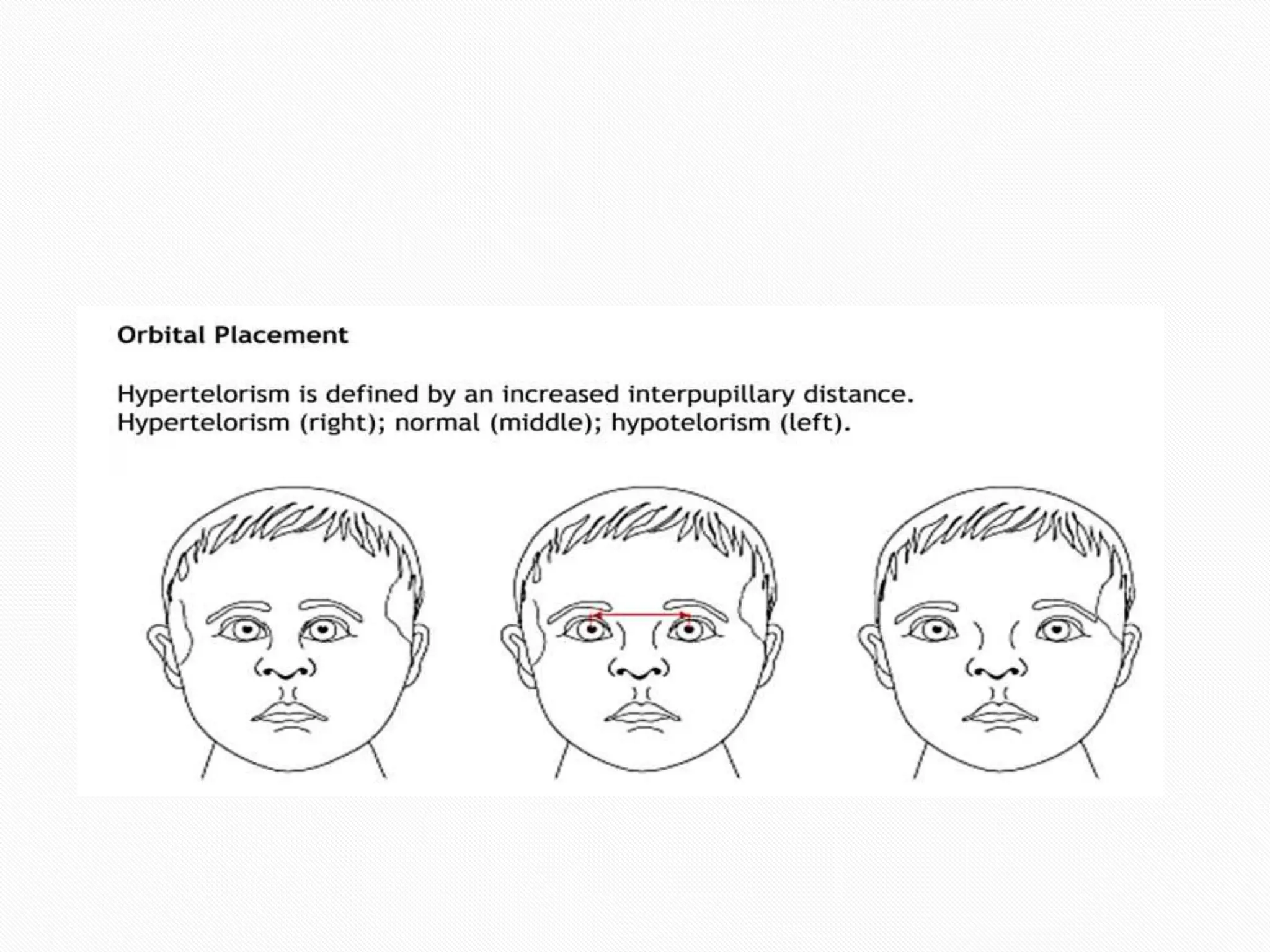
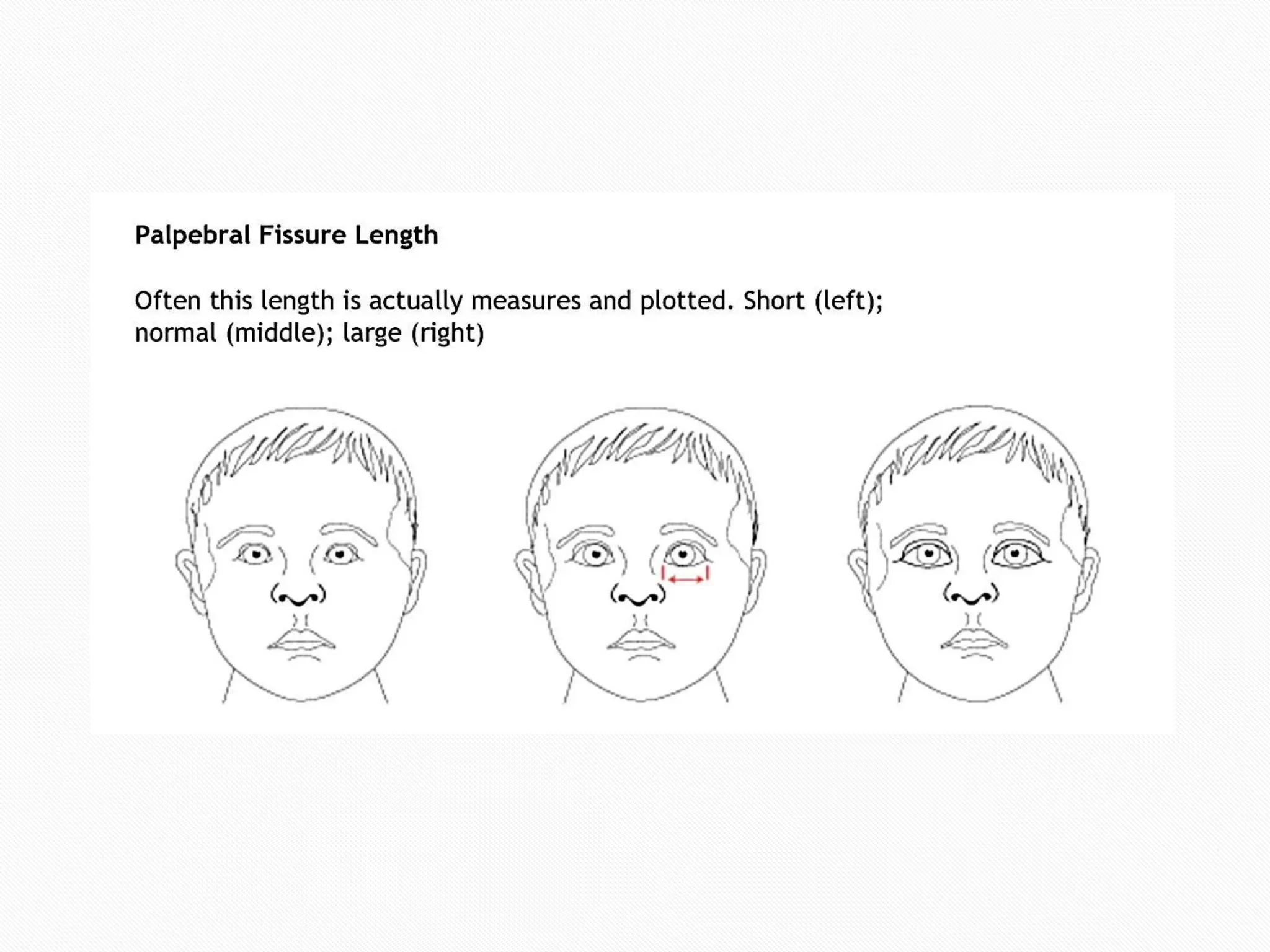
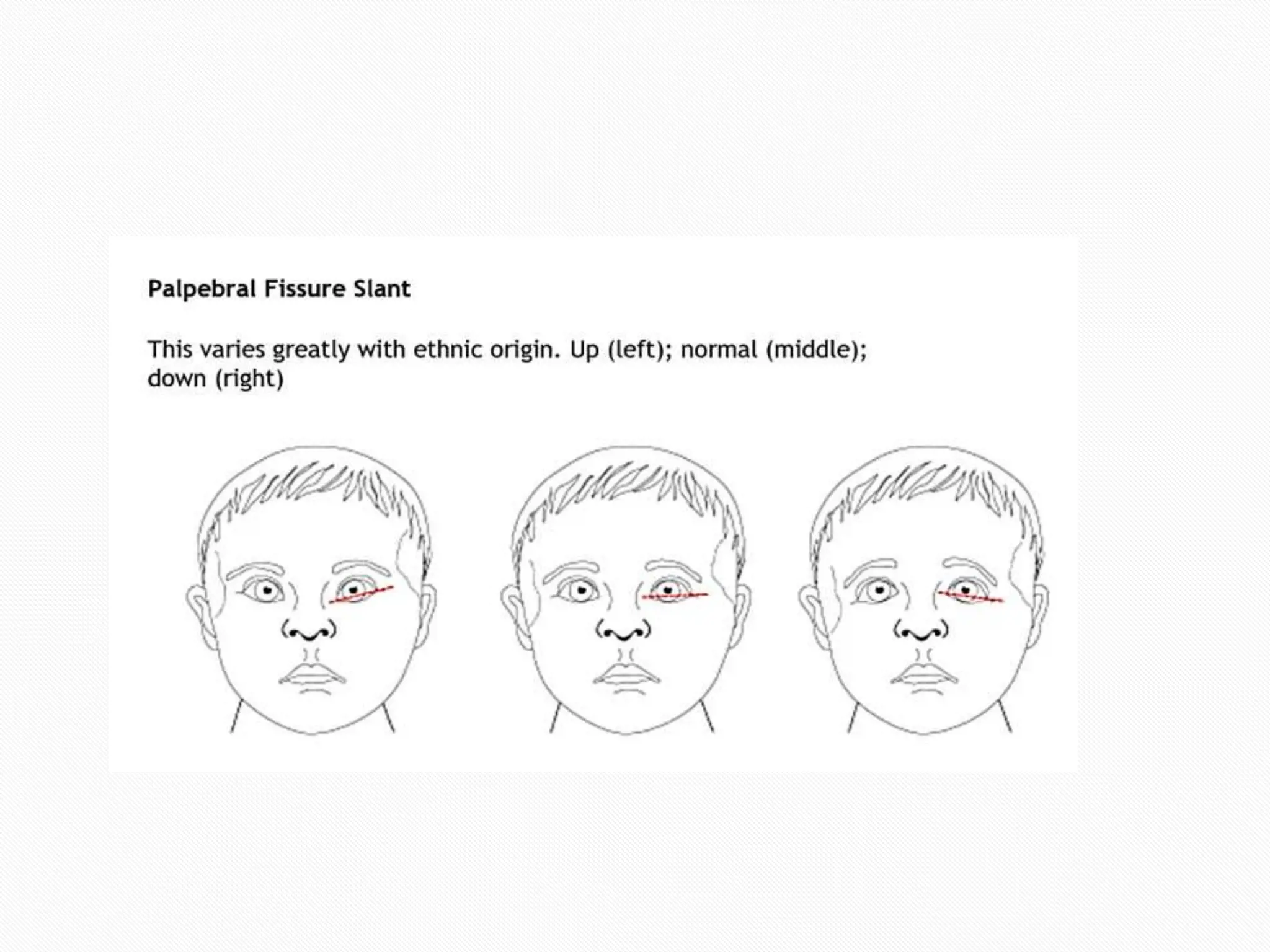
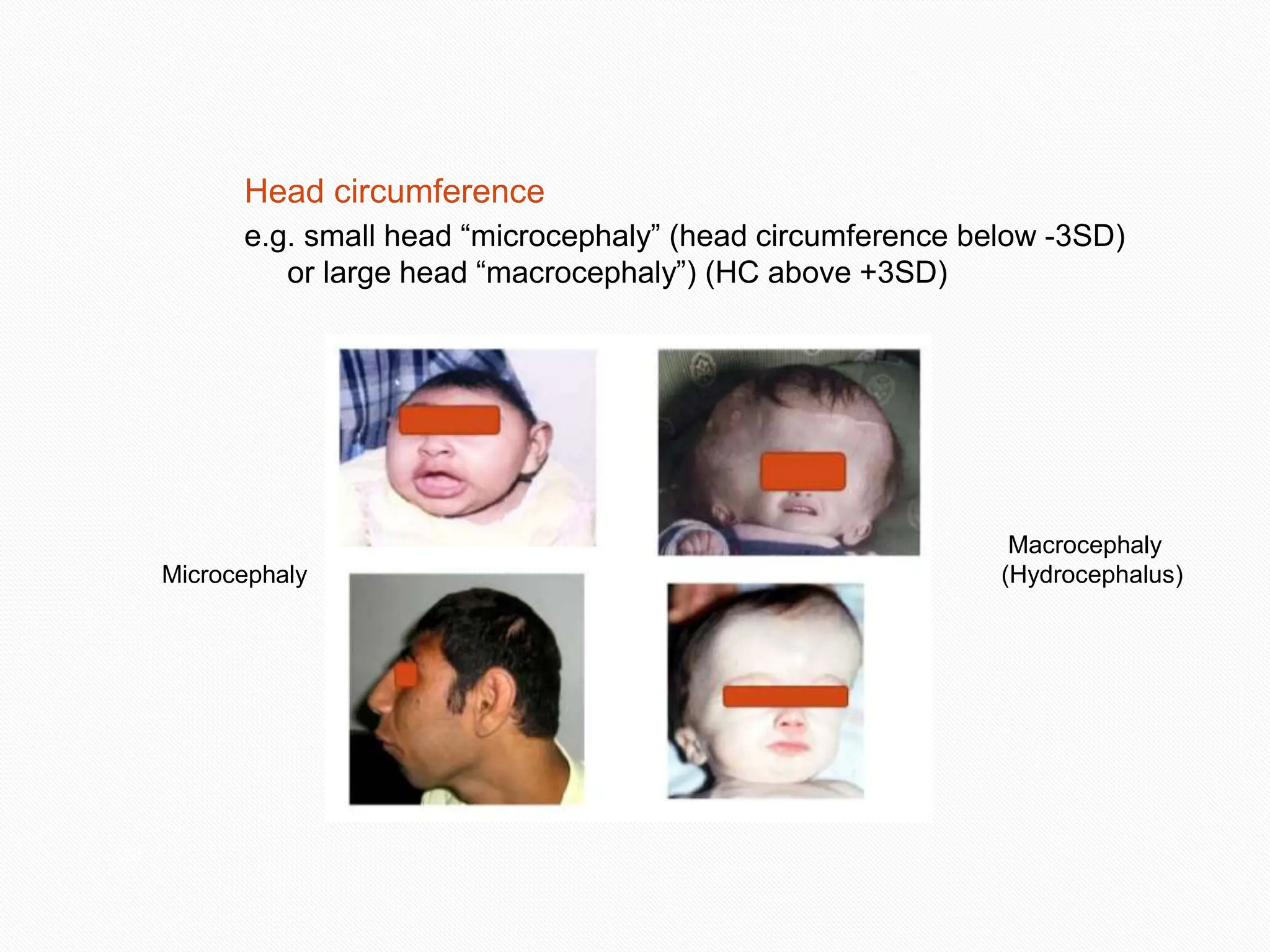
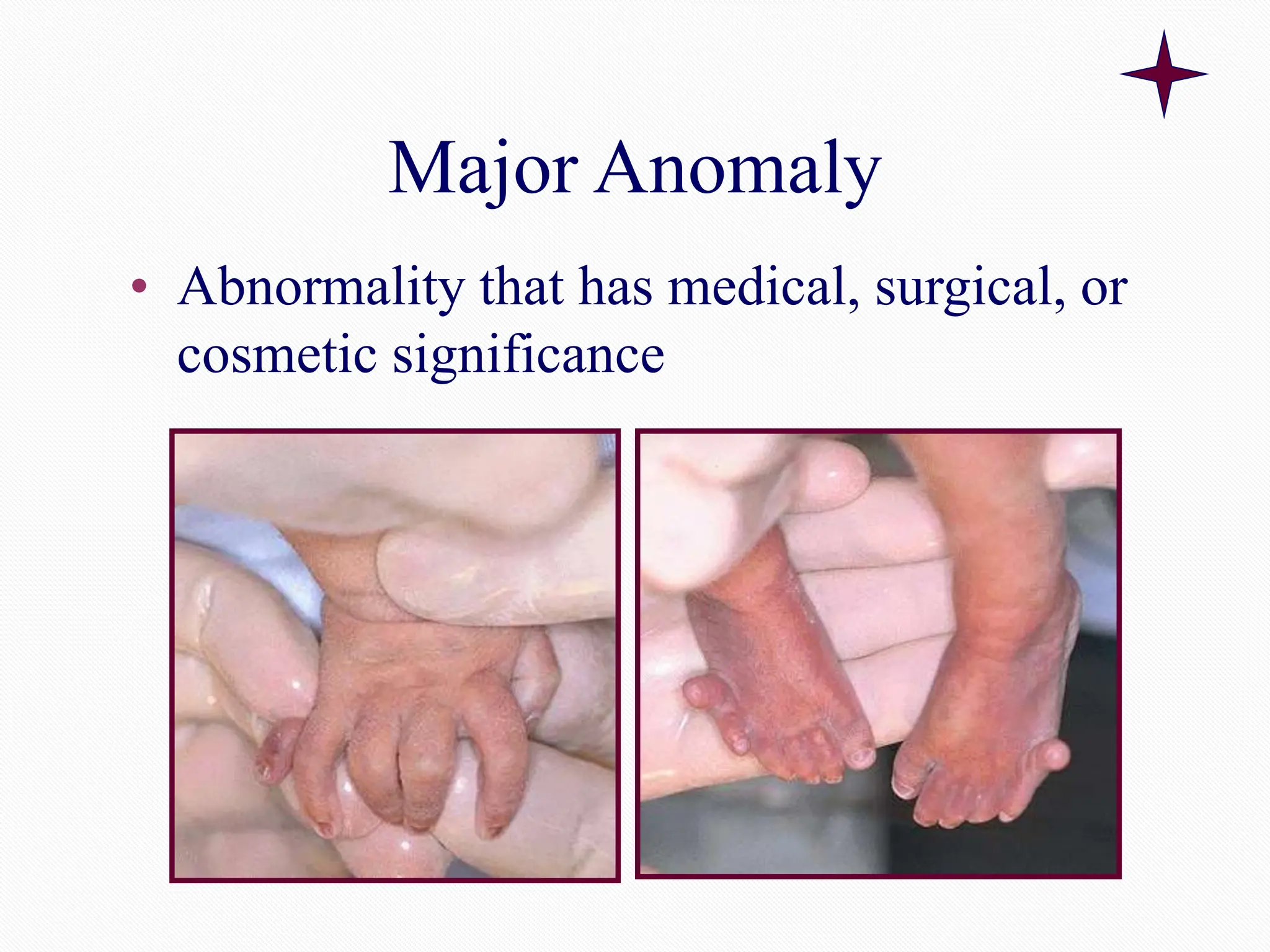
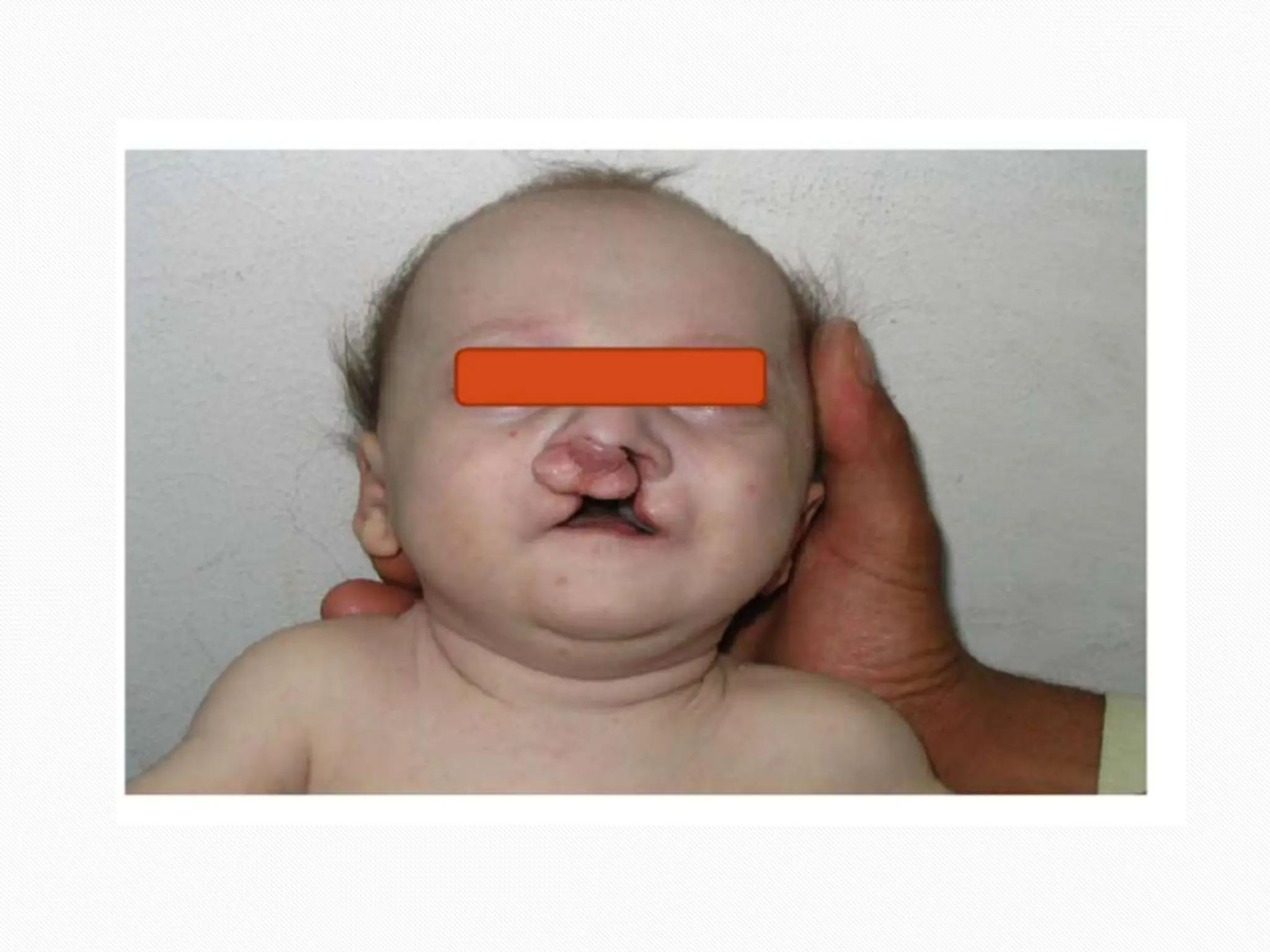
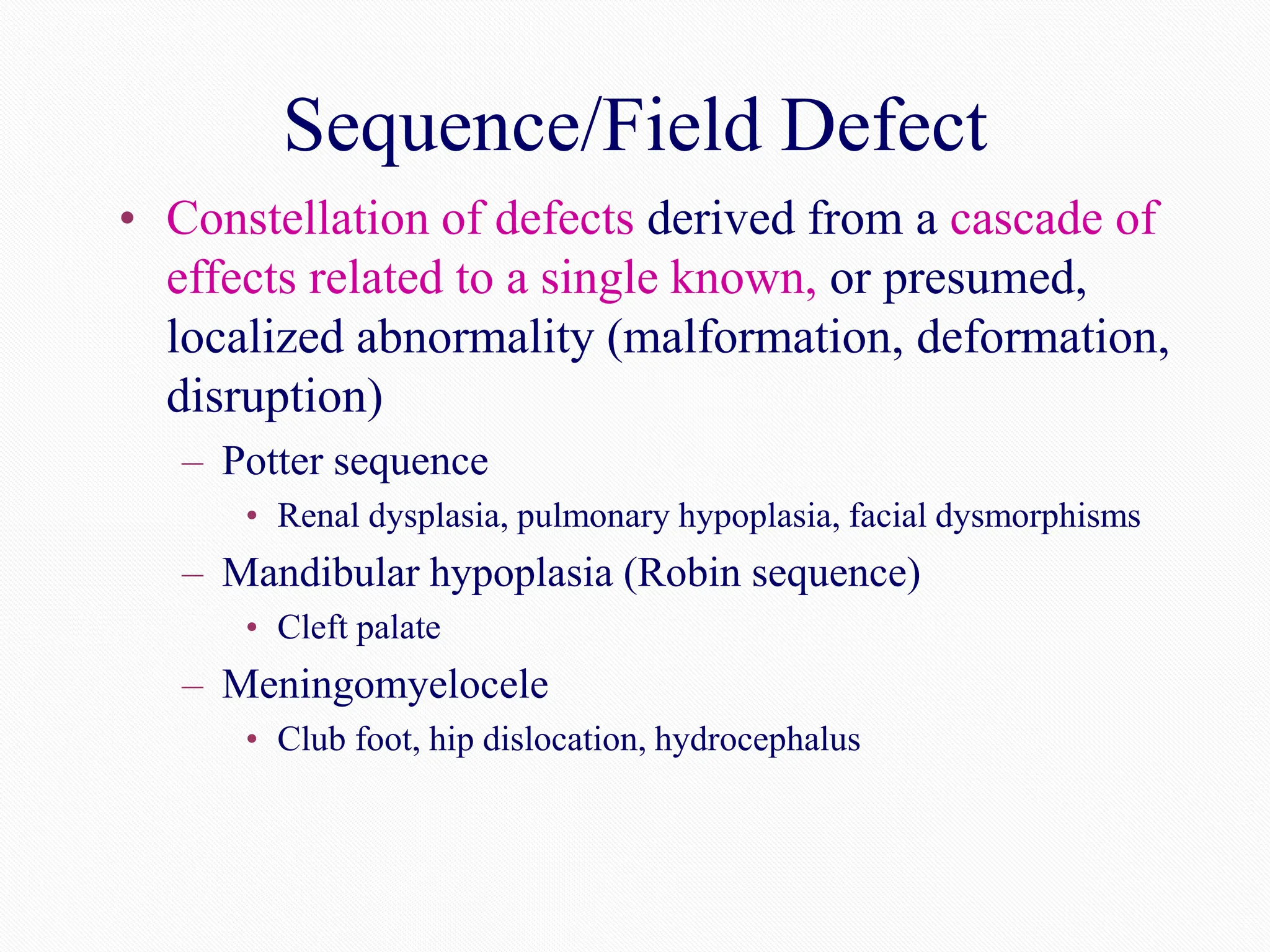
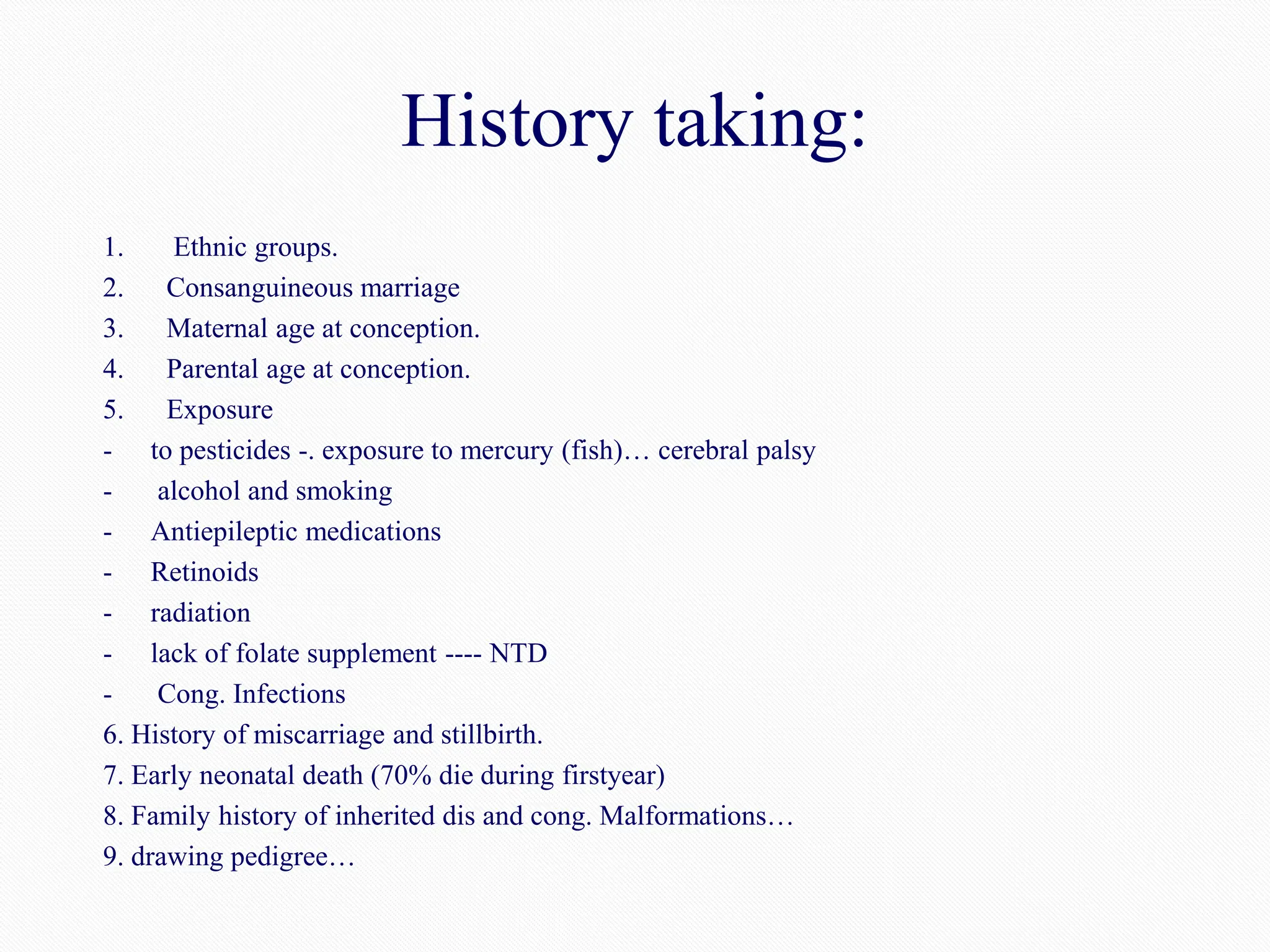
The document discusses dysmorphology, its definition, the impact of birth defects on health, and the classification and causes of congenital anomalies. It emphasizes the importance of a systematic examination and genetic counseling to aid diagnosis and management of patients with dysmorphic features. Key concepts include types of morphogenesis errors, identification of syndromes and associations, and the role of family history in assessing genetic risks.