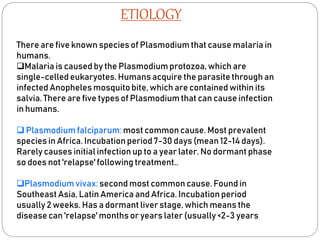
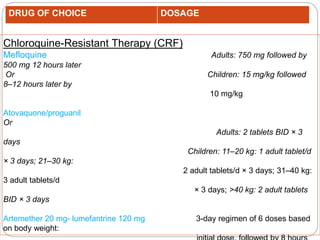
Malaria is a life-threatening illness caused by the Plasmodium protozoa, transmitted through bites from infected Anopheles mosquitoes. It is endemic in many tropical areas, particularly in India, with significant morbidity and mortality rates, prompting global health targets aimed at reducing malaria incidence significantly by 2030. Diagnosis involves various methods such as blood smears and rapid tests, while treatment requires timely anti-malarial therapy, with pharmacological options differing based on the species of Plasmodium involved.












![Monitoring :
BLOOD GLUCOSE[ 4 HOURLY]
HAEMOGLOBIN
CREATININE
CLOTTINGPROFILE
ELECTROLYTES
DAILYPARASITECOUNT](https://image.slidesharecdn.com/presentationonmalaria1-1-231108051103-fdcfc090/85/MALARIA-16-320.jpg)



