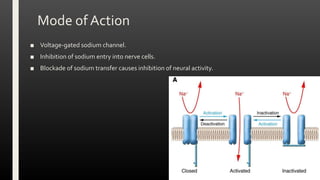
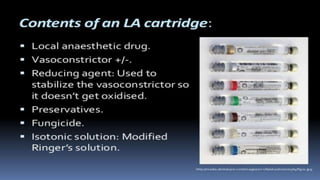
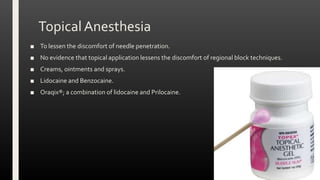
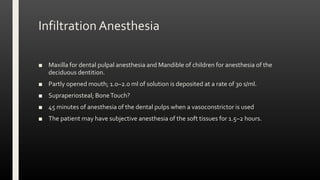
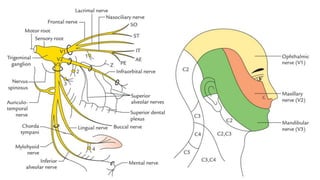
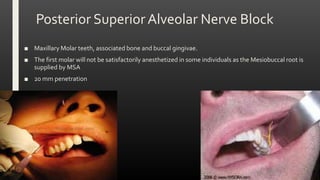
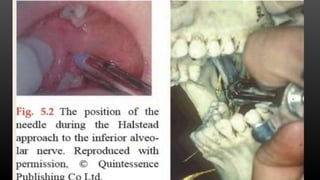
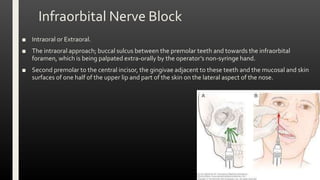
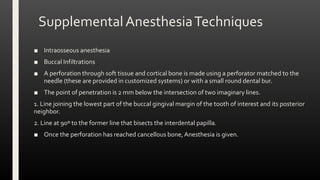
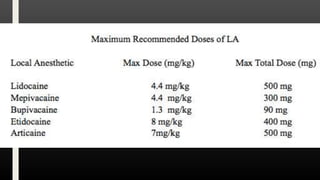
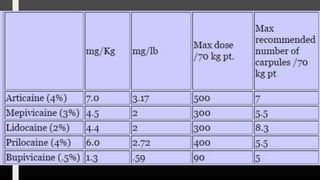
This document provides an overview of local anesthesia including its mode of action, techniques, drugs, and complications. It discusses how local anesthetics work by blocking sodium channels and inhibiting neural activity. Various regional block techniques are described for anesthetizing nerves like the inferior alveolar nerve and maxillary nerve. Common drugs used include lidocaine, mepivacaine, prilocaine, and bupivacaine. Potential complications include nerve damage, motor paralysis, trismus, and systemic issues like allergy or toxicity.