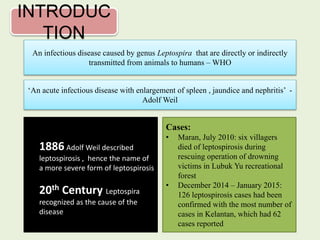
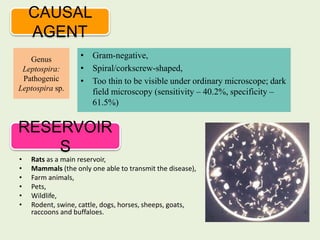
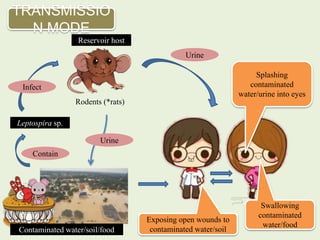
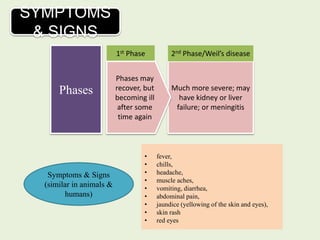
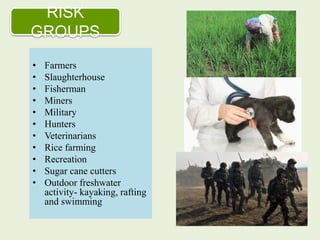
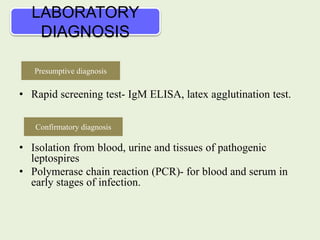
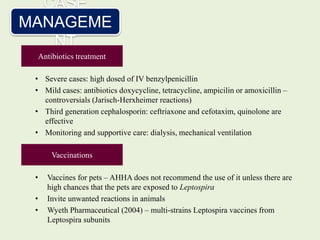
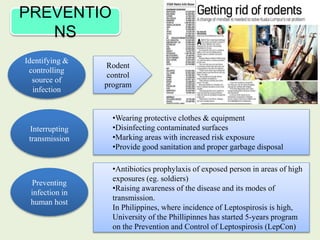
Leptospirosis, an infectious disease caused by the genus Leptospira, is transmitted from animals to humans, primarily through contaminated water and urine from rats and other mammals. Significant outbreaks occurred in Malaysia, including the deaths of six villagers in 2010 and 126 confirmed cases from December 2014 to January 2015. Prevention strategies include controlling rodent populations, using protective equipment, and raising public awareness, with vaccination being recommended only in high-risk situations.