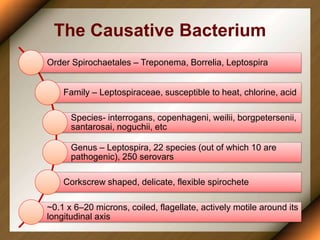
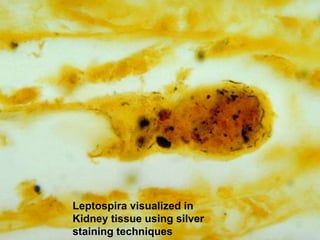
Leptospirosis is a zoonotic disease caused by bacteria of the genus Leptospira. It was first described in 1886 and the causative organism was identified in 1907-1908. It commonly affects those exposed to contaminated water or soil, especially in tropical regions with high rainfall. Clinical presentation ranges from a mild flu-like illness to a severe form called Weil's disease involving jaundice, renal failure and hemorrhage. Diagnosis is difficult due to non-specific symptoms but can be confirmed through microscopic agglutination testing of blood samples taken during the immune phase. Prompt treatment with antibiotics is important for severe cases to reduce mortality.