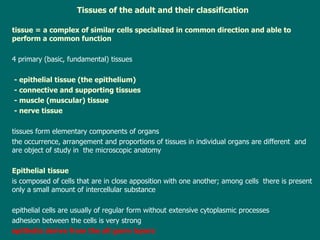
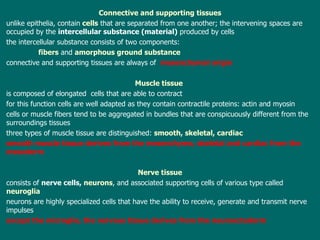
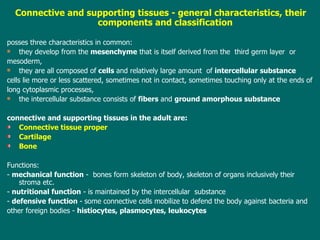
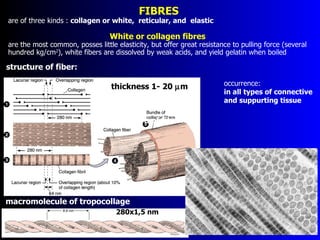
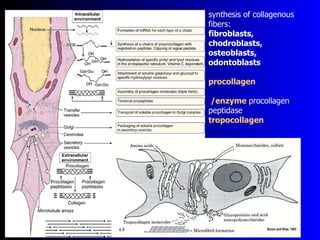
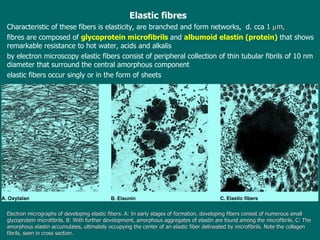
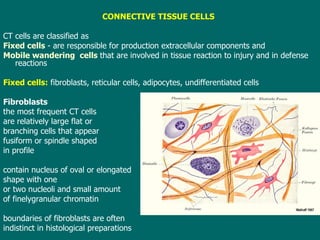
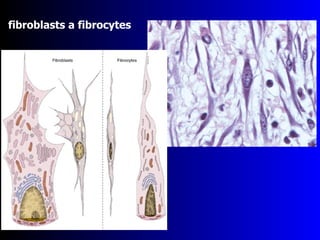
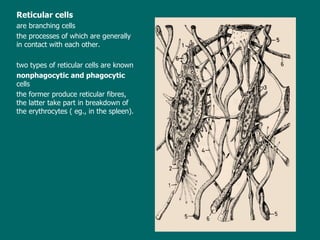
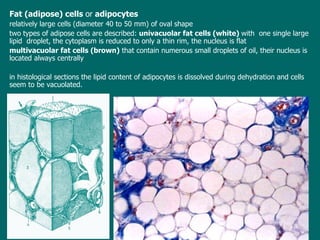
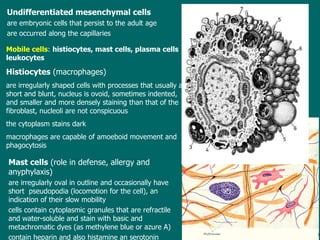
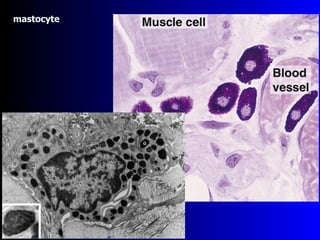
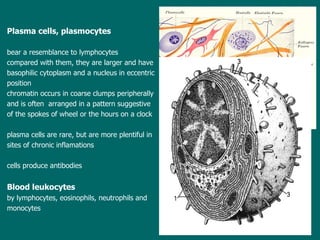
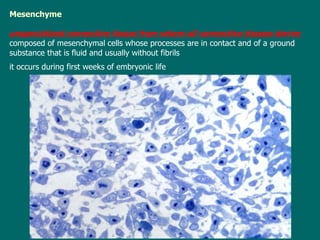
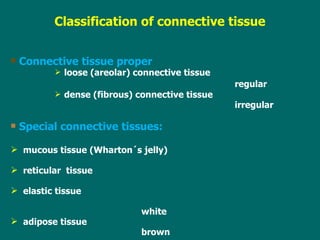
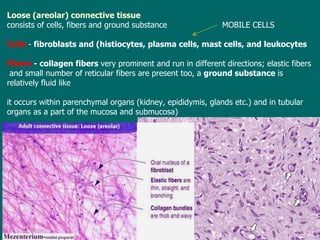
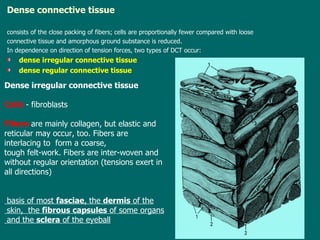
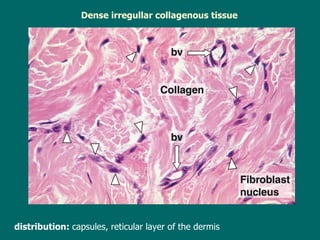
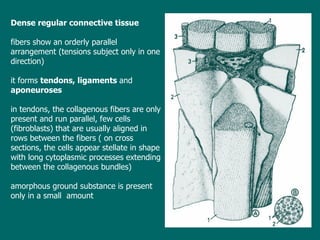
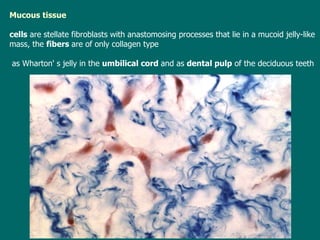
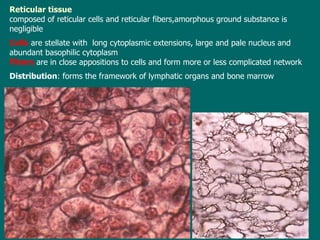
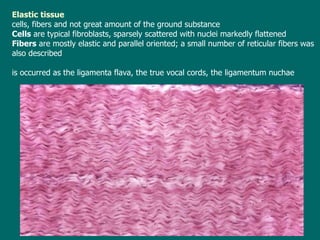
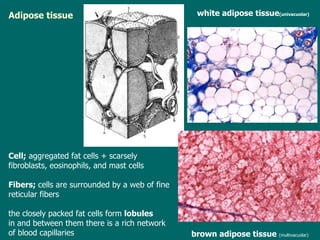
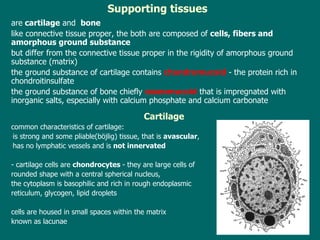
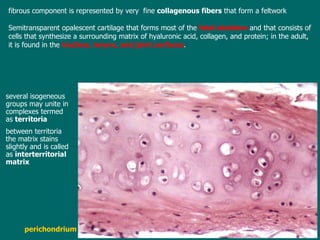
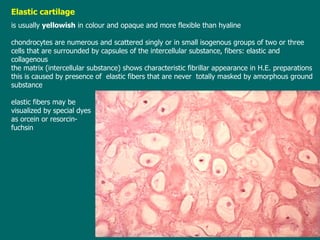
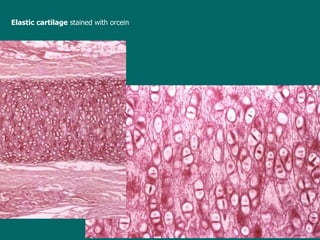
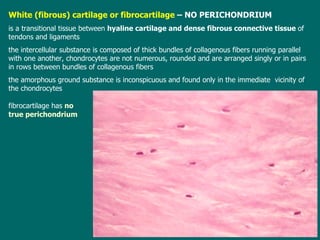
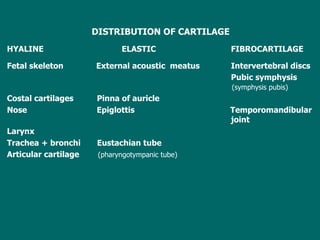
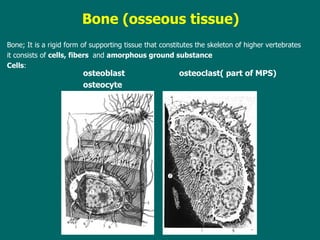
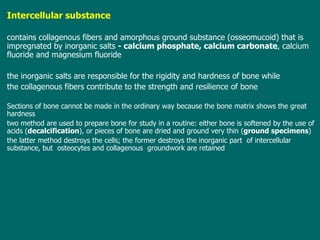
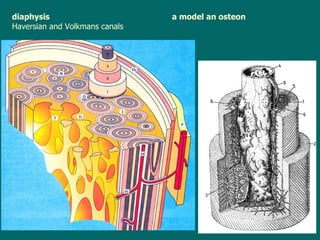
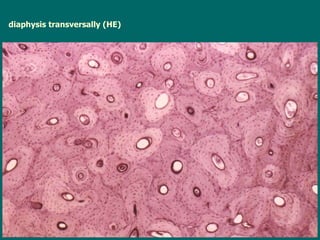
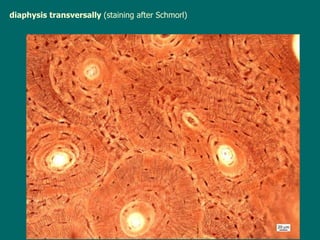
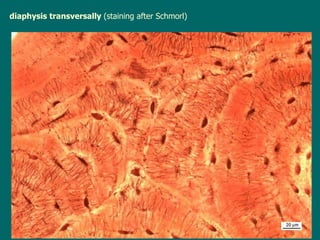
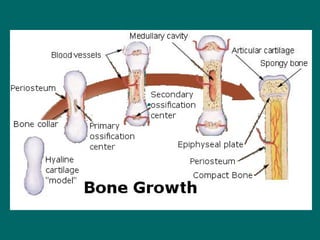
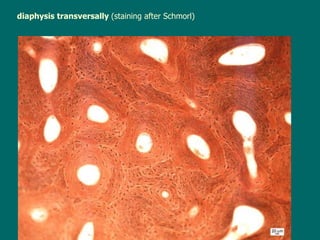
The document defines and classifies tissues and connective tissue. It discusses the four primary tissues - epithelial, connective, muscle and nerve tissue. Connective tissue contains cells separated by intercellular substance composed of fibers and ground substance. Three fiber types are described - collagenous, reticular, and elastic. Connective tissue cells include fixed cells like fibroblasts and adipocytes, and mobile cells involved in tissue reactions and defense. Bone and cartilage are described as supporting tissues that develop from mesenchyme.