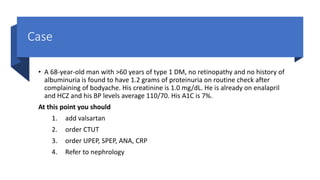
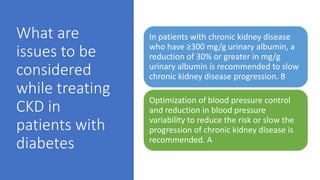
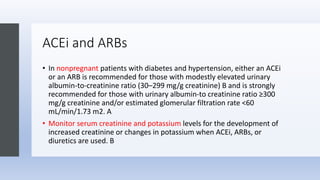
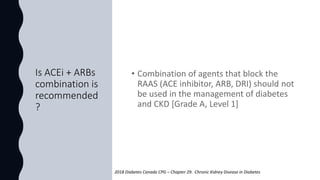
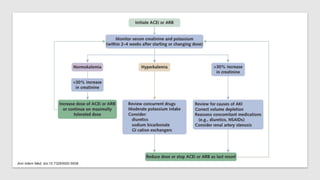
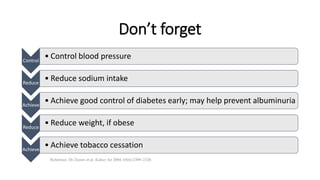
No, the combination of an ACE inhibitor and an ARB is not generally recommended for patients with diabetes and CKD. Some key points:
- There is no evidence that combining an ACEi with an ARB provides additional renal protection compared to monotherapy in patients with diabetes and CKD.
- Combining the two classes of drugs increases the risk of hyperkalemia and acute kidney injury without proven additional benefit over monotherapy.
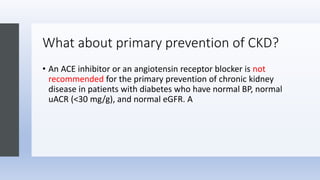
- Current guidelines recommend using either an ACEi or an ARB as first-line therapy for albuminuria, but do not recommend combining the two classes of drugs.
So in summary, while ACEis and ARBs are both reasonable first-line options, combining