This document discusses juvenile idiopathic arthritis (JIA), including:
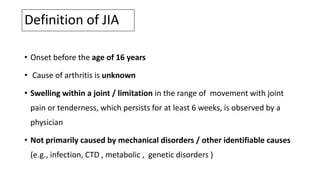
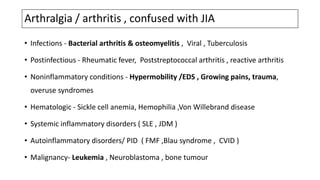
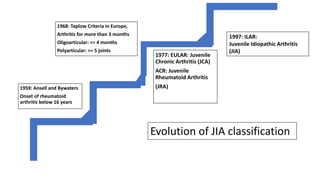
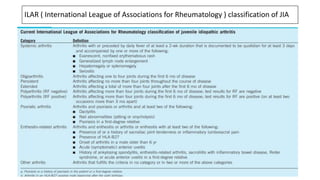
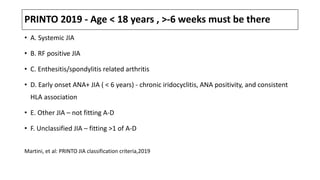
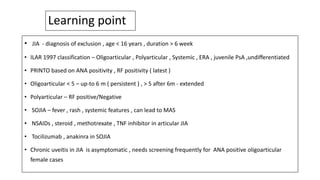
1. It defines JIA and differentiates it from other causes of arthritis in children.
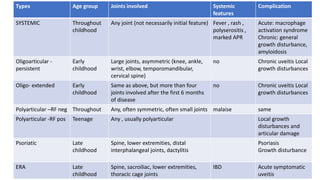
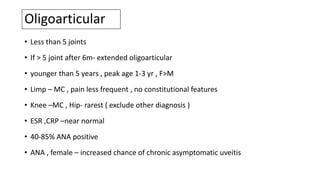
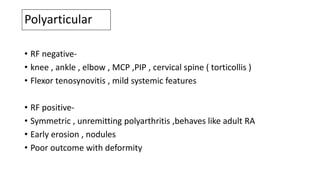
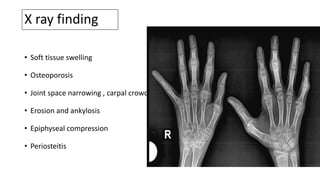
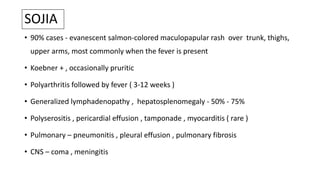
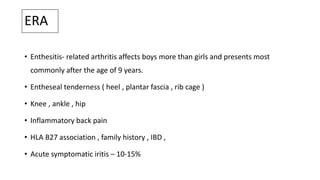
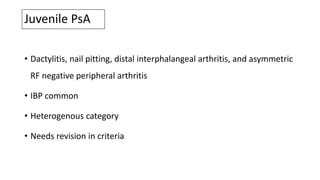
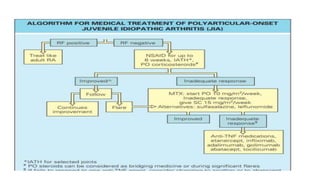
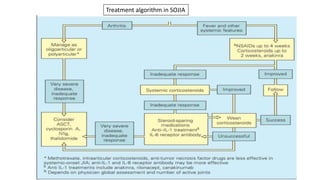
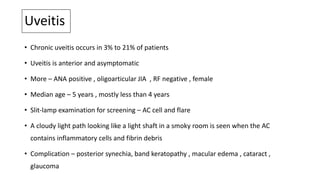
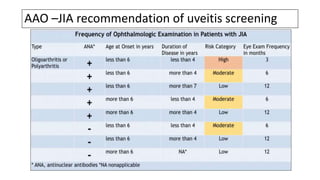
2. It describes the different subtypes of JIA based on number of joints involved, presence of systemic features, and other characteristics.
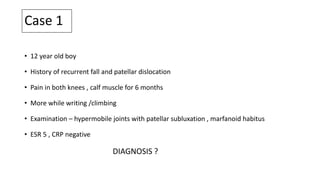
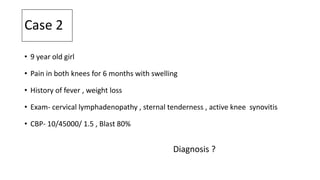
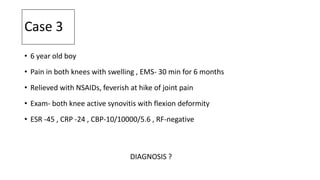
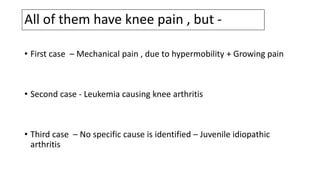
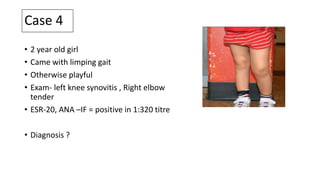
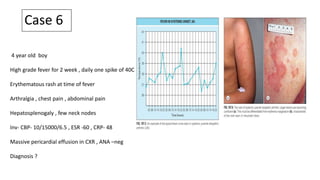
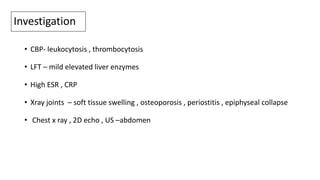
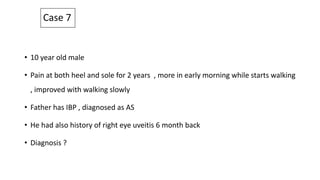
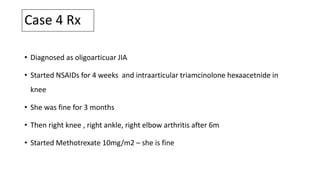
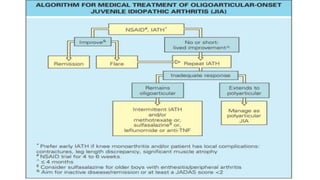
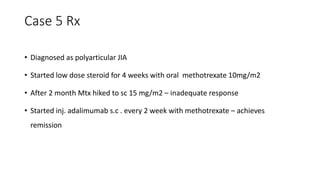
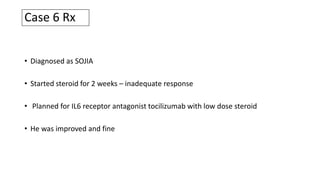
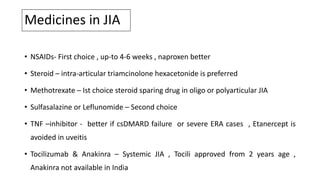
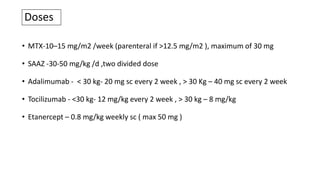
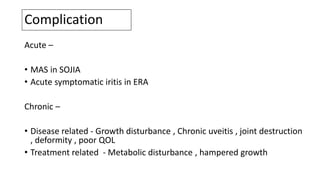
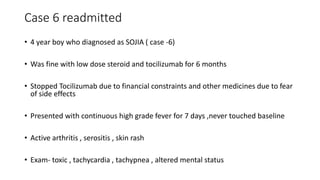
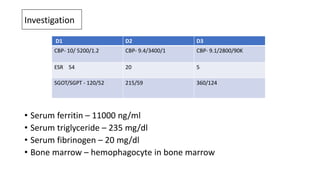
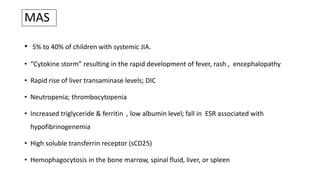
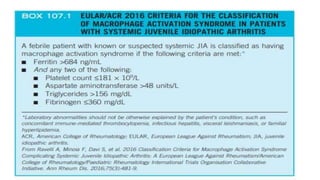
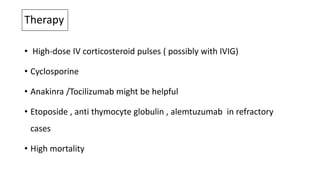
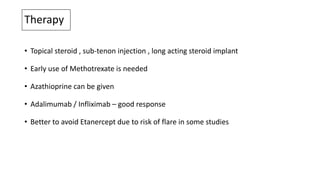
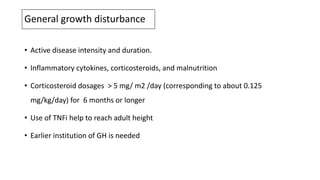
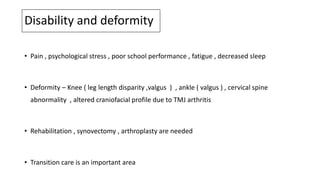
3. It discusses the clinical features, investigations, treatment approaches, and complications of JIA through several case examples.