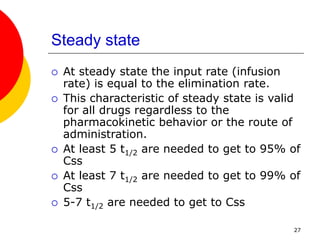
The document discusses one-compartment pharmacokinetic models for intravenous bolus and continuous infusion drug administration. For an IV bolus, drug concentration declines exponentially over time according to the one-compartment model equation. A short infusion can be modeled as a bolus if the infusion time is small relative to the drug half-life. For continuous IV infusion, drug concentration reaches a steady state level determined by the infusion rate and drug clearance. Pharmacokinetic parameters like elimination rate constant, volume of distribution, and clearance can be estimated from concentration-time data using the one-compartment model equations.