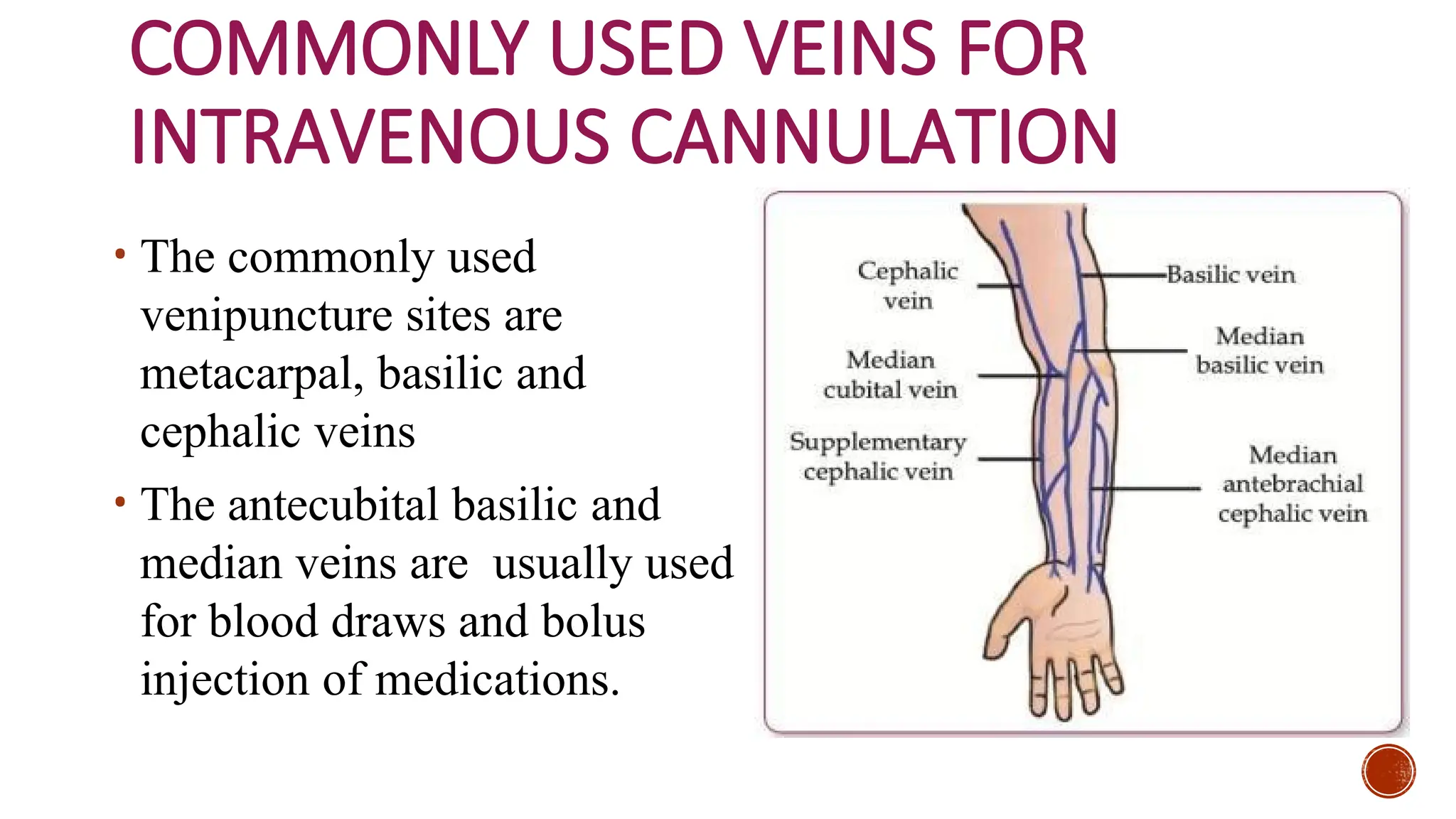
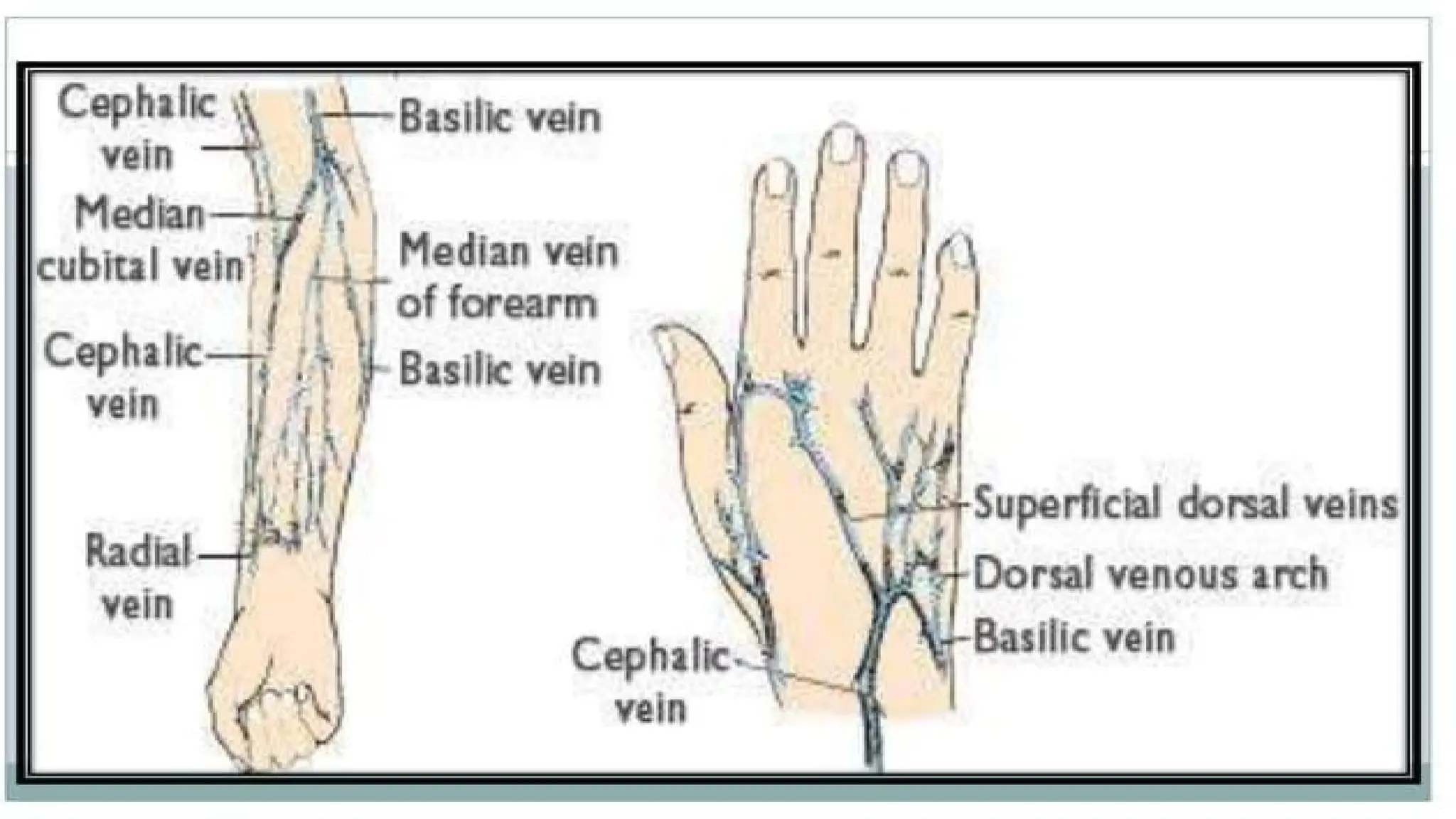
The document provides an overview of intravenous (IV) therapy, detailing its purpose, types of IV fluids, and procedures for cannulation, as well as highlighting potential local and systemic complications. It categorizes IV fluids into crystalloid and colloid solutions based on solute concentration and discusses factors influencing site selection for cannulation. Additionally, it emphasizes the importance of measuring and monitoring fluid intake and output to maintain fluid and electrolyte balance in patients.