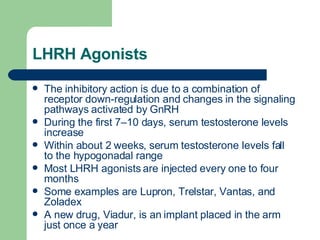
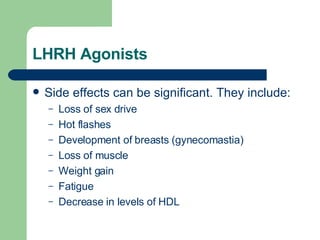
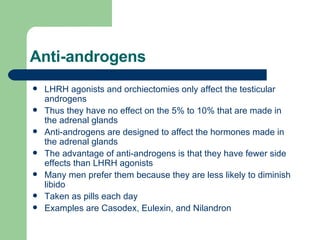
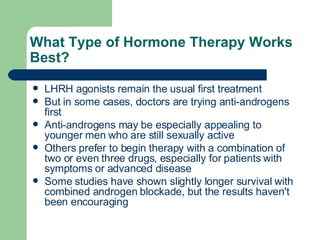
Hormonal therapy for prostate cancer is effective in 80-90% of advanced cases, primarily through androgen deprivation techniques. Various hormonal therapies exist, including LHRH agonists and anti-androgens, with some approaches combining both to enhance efficacy while managing side effects. The choice of therapy may vary based on patient status and preferences, and there is ongoing debate regarding the timing and combination of treatments.