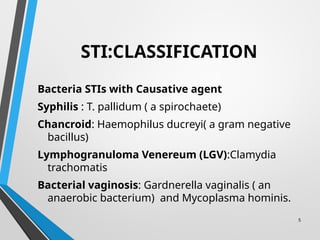
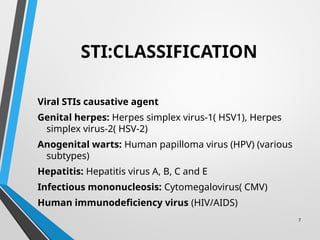
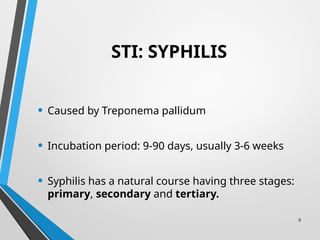
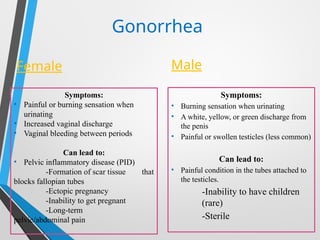
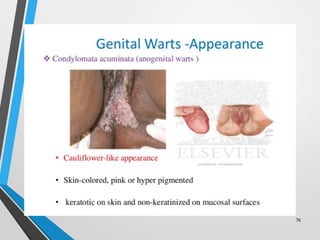
The document outlines details about sexually transmitted infections (STIs), with a focus on syphilis, gonorrhea, and chancroid, including their causes, symptoms, classifications, and treatment options. It highlights the transmission methods, risks associated with multiple sexual partners, and complications that can arise if left untreated, particularly concerning pregnancy. Additionally, the document provides diagnostic methods and preventative measures for managing these infections.