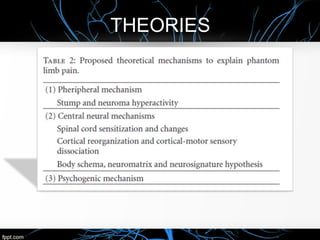
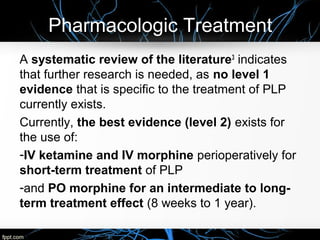
This document discusses phantom limb pain (PLP), a condition where amputees experience pain in the region of a limb that is no longer present. It provides a brief history of PLP and notes that its pathophysiology and treatment remain poorly understood. Several potential mechanisms are discussed, including peripheral, central, and psychological factors. Current best evidence supports the short-term use of IV ketamine/morphine and long-term oral morphine for PLP treatment. Non-pharmacological options mentioned include TENS, mirror therapy, acupuncture, and myoelectric virtual reality systems that respond to muscle activity in the remaining limb stump. Further research is still needed to better understand PLP and develop more effective treatments.