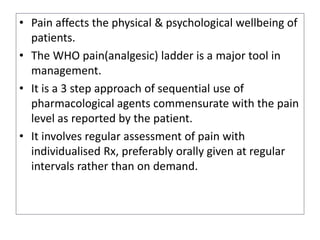
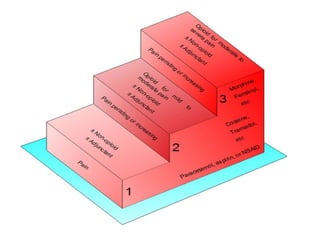
The document discusses intra and postoperative analgesia. It begins by providing background on the history of pain relief before the 19th century and the first public uses of ether as anesthesia. It then covers the anatomy and physiology of pain transmission and nociception. The bulk of the document focuses on the World Health Organization's pain ladder approach for managing pain, moving sequentially from non-opioid and weak opioid options in mild pain up to strong opioids for severe pain. Specific analgesic drugs are discussed at each step, along with adjuvant therapies and methods of administration like patient-controlled analgesia.



![Transmission of impulses from
nociceptors
• Impulses are transmitted to the CNS via two fibre types:
– Thinly myelinated A-delta fibres [found in hairy and glabrous skin and
deep tissue]
– Unmyelinated C fibres which conduct at lower rates.
• Activation of A-delta fibre which release glutamate, is
responsible for first pain(fast pain), a rapid response and
mediates the discriminative aspect of pain (the ability to
localize the site and intensity of the noxious stimulus).
• Activation of C fibre, release a combination of glutamate and
substance P, and is responsible for delayed second pain (slow
or protopathic pain) which is dull, intense, diffuse, and
unpleasant feeling associated with a noxious stimulus.](https://image.slidesharecdn.com/intrapostopanalgesiappt-200416141245/85/Intra-amp-post-op-analgesia-ppt-7-320.jpg)