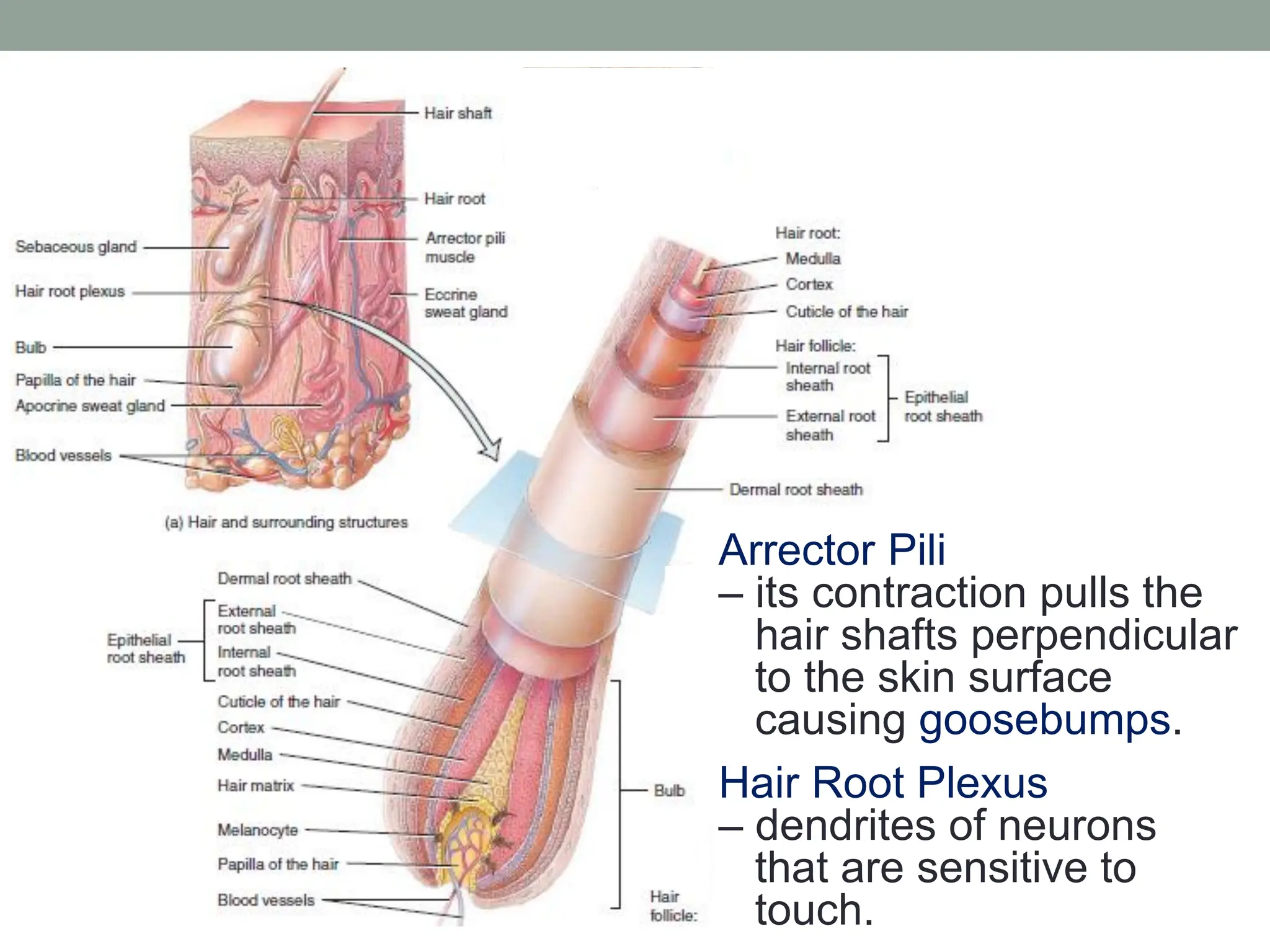
The integumentary system comprises the skin and its accessory structures, providing crucial functions such as temperature regulation, protection, sensation, and vitamin D synthesis. The skin is layered into the epidermis and dermis, with various cell types, each having specific roles in protection, sensation, and pigmentation. Accessory structures like hair, nails, and glands support skin functions and contribute to overall homeostasis.