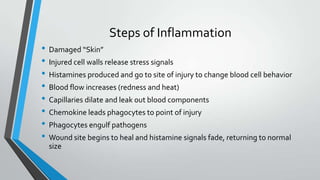
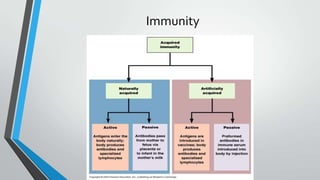
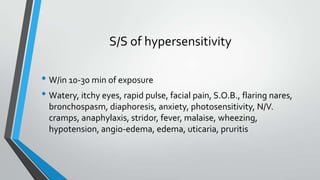
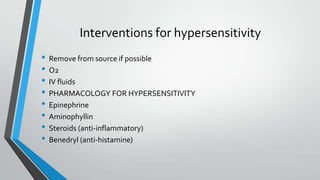
This document summarizes inflammation, the immune response, infections, and hypersensitivity reactions. It describes the steps of acute and chronic inflammation. It also discusses the functions of the immune system, signs and symptoms of infection, immunity, types of infections, nosocomial infections, superinfections, antibiotic-resistant bacteria, and the signs and treatments of hypersensitivity reactions and anaphylaxis. Pharmacological interventions for various conditions are also mentioned.