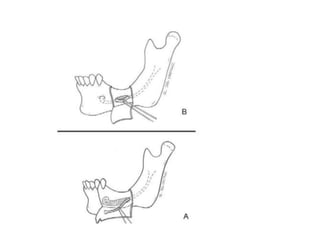
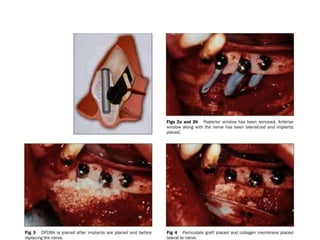
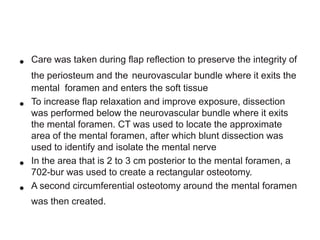
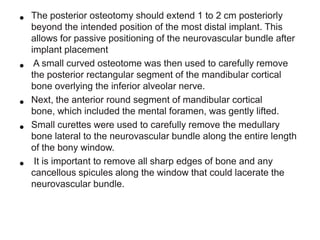
Progressive bone resorption after tooth loss can leave inadequate bone height for dental implants without risking nerve injury. This document describes a technique for repositioning the inferior alveolar nerve laterally to allow safe implant placement medial to the nerve. The procedure involves creating bone windows around the mental foramen and posteriorly, carefully retracting the nerve and placing implants. Bone graft and membranes are used to support the nerve in its new position and prevent direct contact with implants.