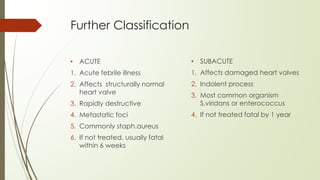
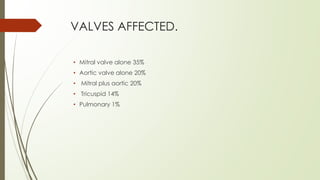
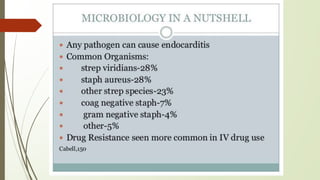
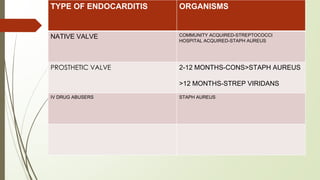
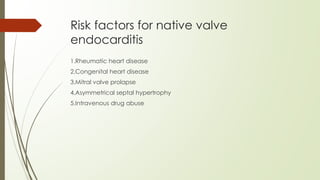
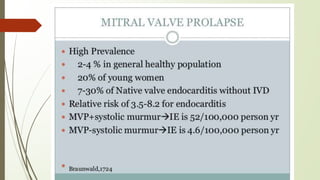
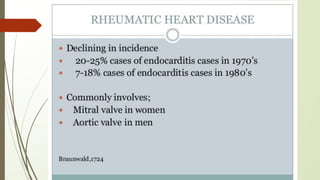
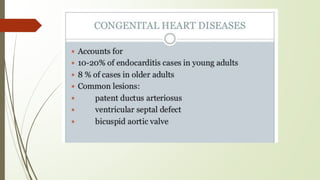
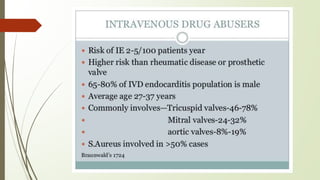
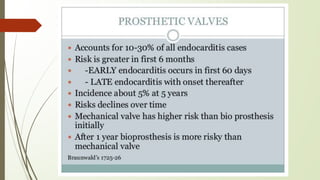
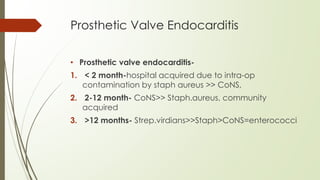
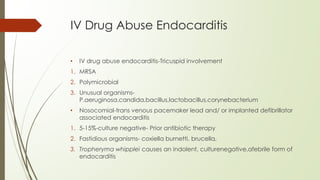
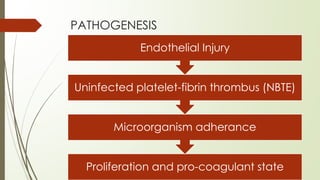
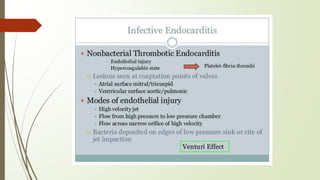
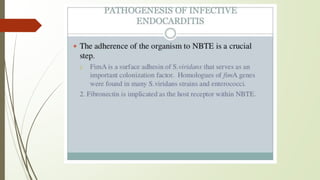
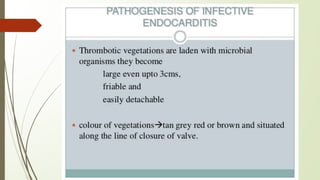
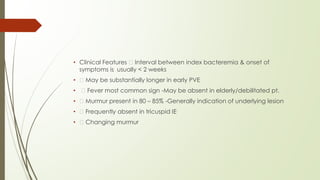
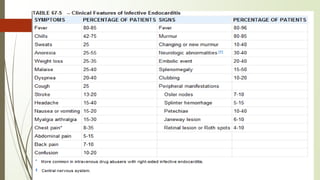
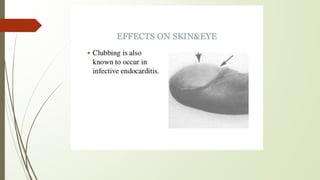
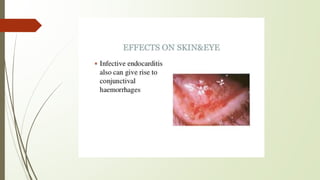
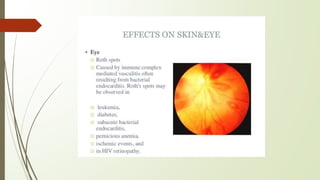
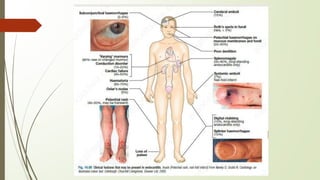
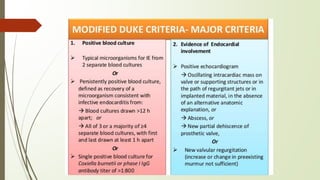
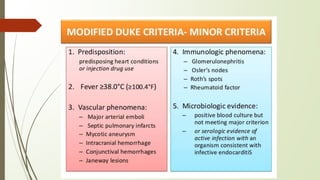
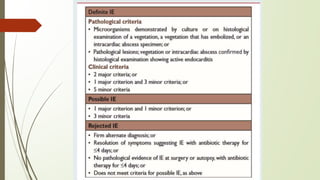
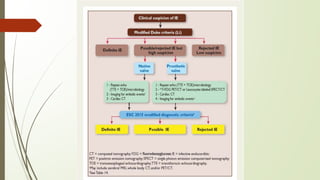
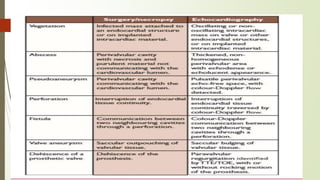
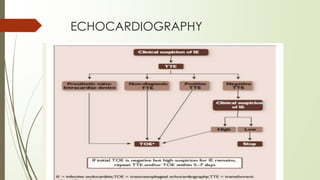
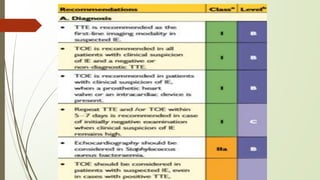
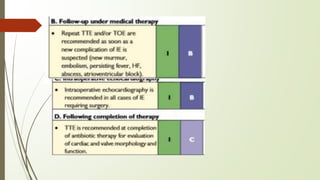
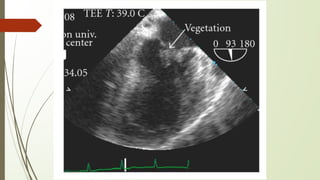
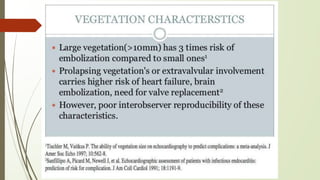
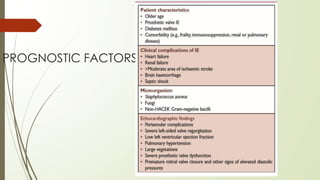
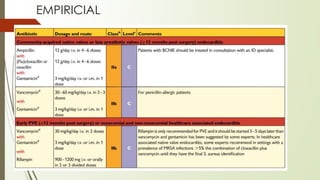
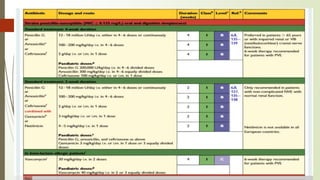
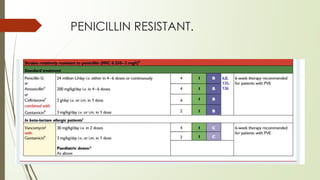
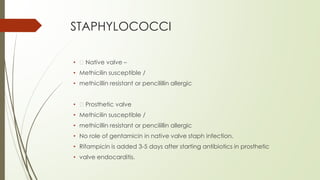
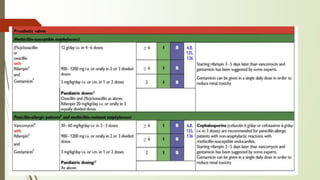
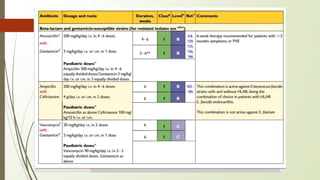
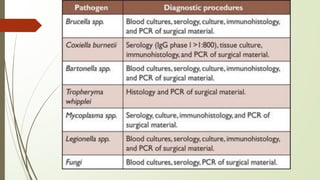
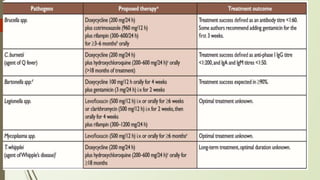
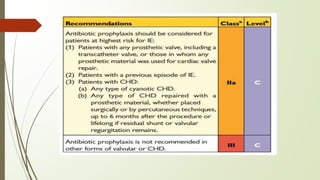
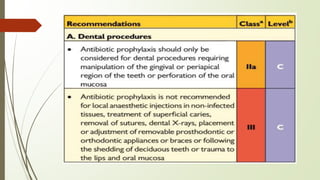
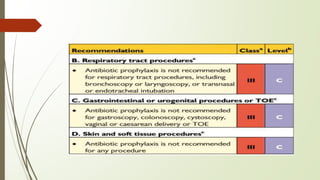
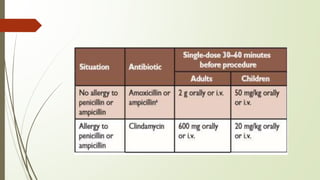
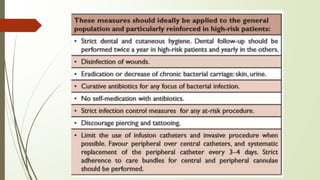
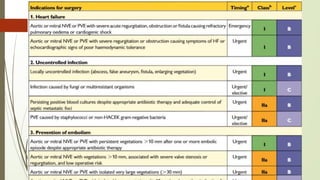
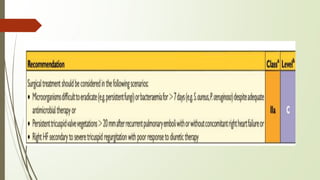
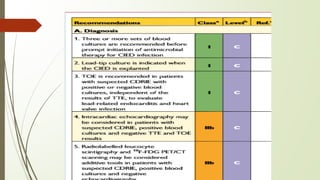
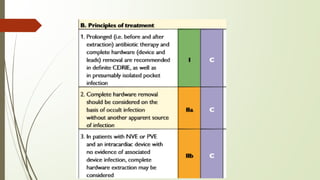
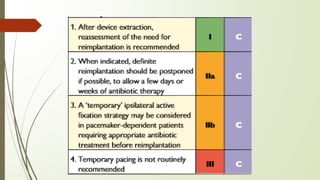
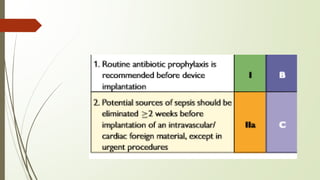
This document provides an overview of infective endocarditis. It defines infective endocarditis as a microbial infection of the endothelial heart surface or intracardiac devices. It discusses the epidemiology, classification, pathogenesis, clinical features, diagnostic criteria, investigations, treatment, and prophylaxis of the condition. The most common causes are streptococci, staphylococci and enterococci bacteria. Infective endocarditis can be native or prosthetic valve endocarditis. If left untreated, it can be fatal in 20-100% of cases depending on diagnosis and treatment. Echocardiography is important for diagnosis, and treatment involves antibiotics tailored to the infecting organism.