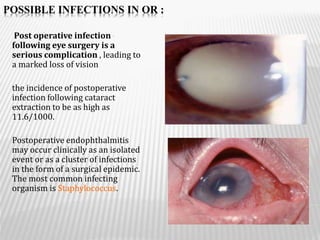
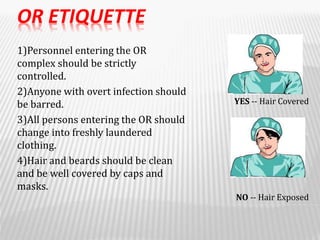
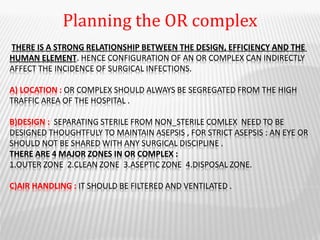
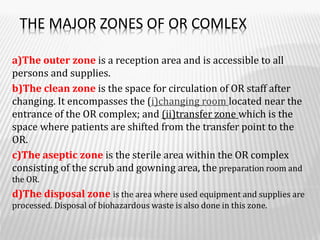
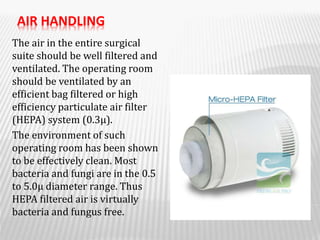
This document discusses infection control practices in operating rooms for ophthalmology. It covers possible infections that can occur, issues with current practices, operating room etiquette, planning and designing the operating room complex layout, caring for instruments, cleaning and sterilization/disinfection of operating rooms. The operating room is the most critical area of the hospital and cleanliness is important for patient safety. A systematic approach by the operating team following proper protocols can help reduce infections.