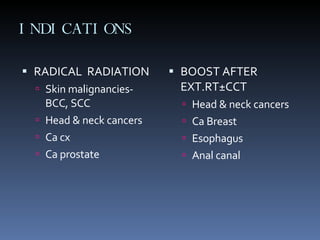
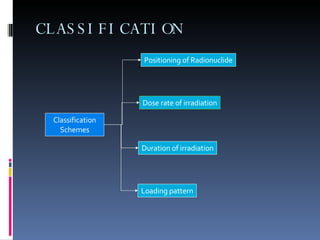
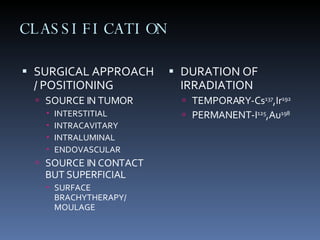
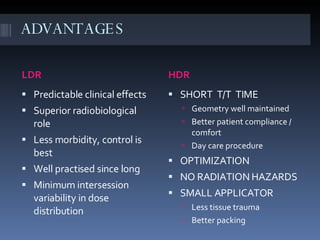
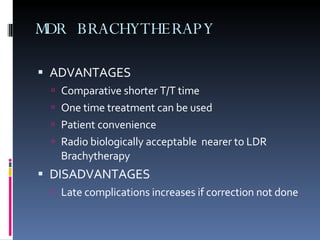
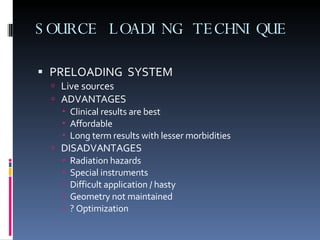
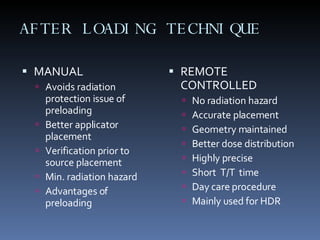
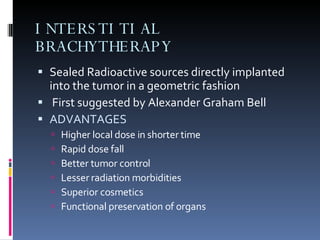
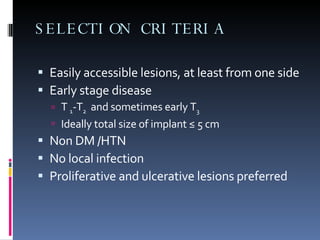
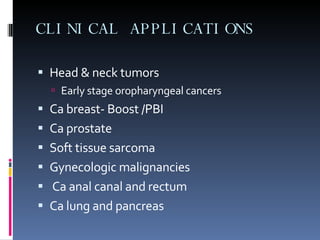
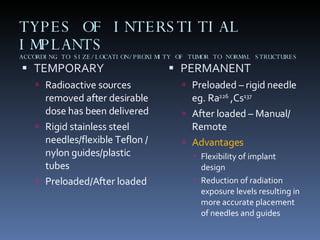
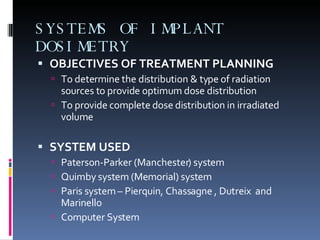
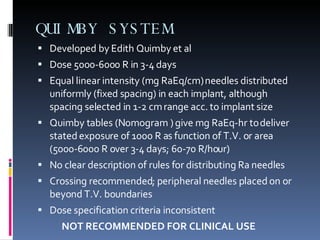
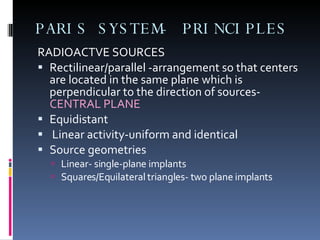
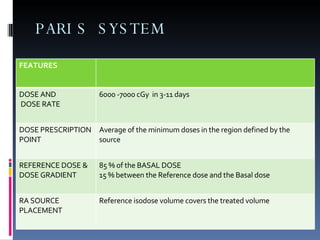
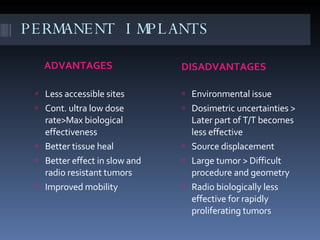
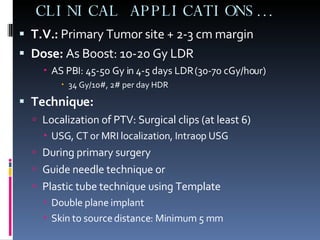
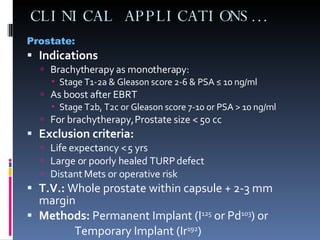
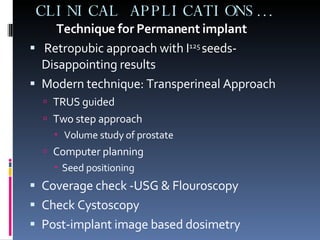
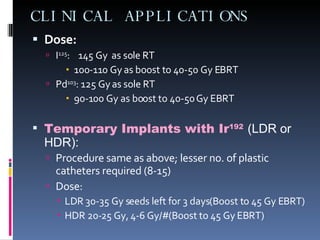
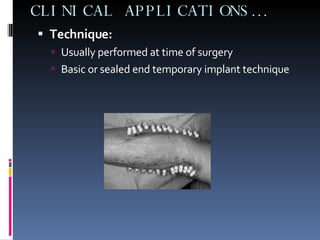
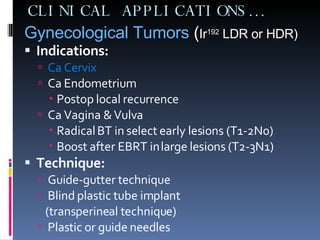
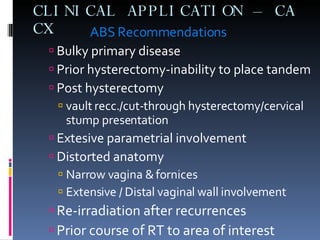
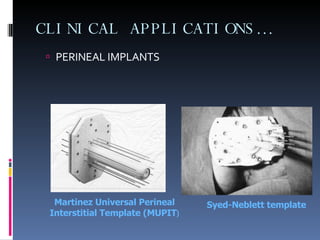
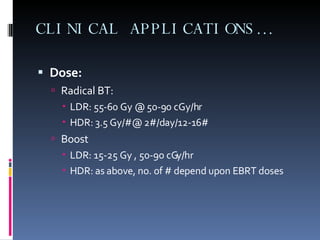
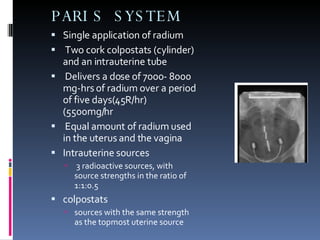
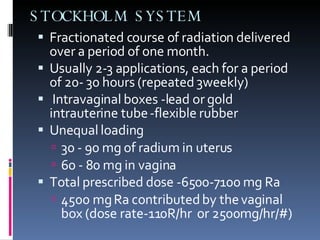
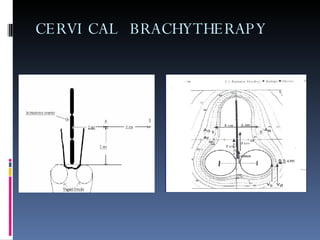
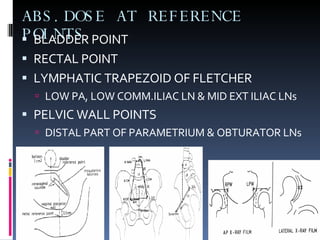
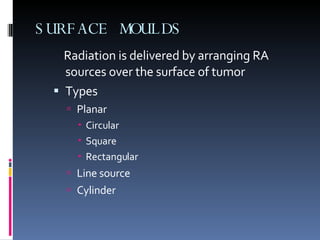
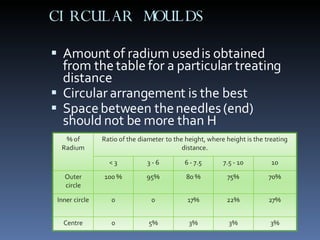
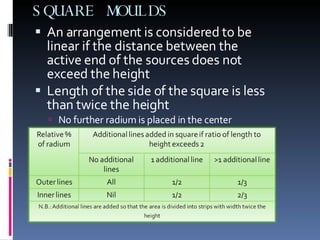
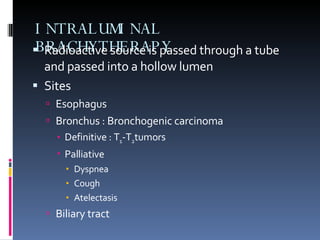
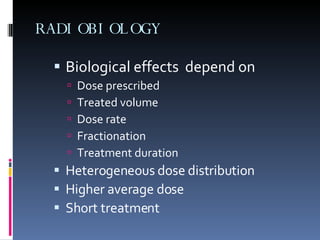
This document provides an overview of brachytherapy including its principles, methods, advantages, limitations, indications, classifications, and clinical applications. Brachytherapy involves placing radioactive sources close to or inside the tumor to deliver a high dose of radiation directly to the tumor with rapid dose fall-off sparing surrounding normal tissues. It discusses various brachytherapy techniques including interstitial, intracavitary, and surface applications for treating cancers of the breast, prostate, head and neck, and soft tissue sarcomas among others.