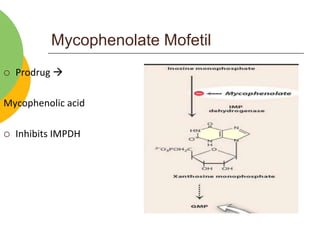
This document discusses immunomodulators, which are drugs that either suppress or stimulate the immune system. It describes various types of immunosuppressants including calcineurin inhibitors like cyclosporine and tacrolimus, mTOR inhibitors like sirolimus, antiproliferative drugs, glucocorticoids, and biological agents. It also discusses immunostimulants such as BCG, cytokines, interferons, and immunoglobulins. The document provides details on the mechanisms of action, uses, and side effects of various immunomodulator drugs.