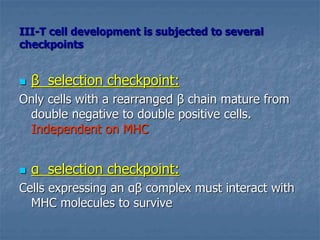
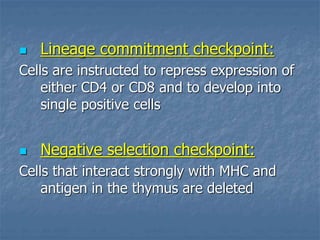
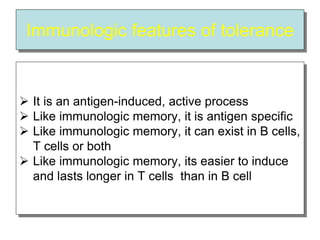
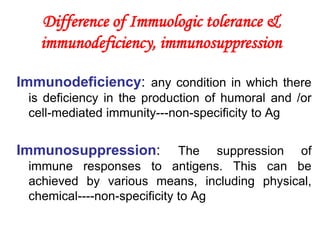
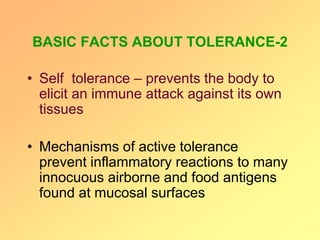
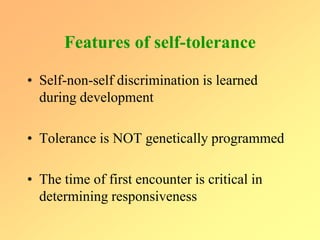
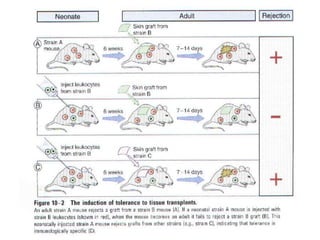
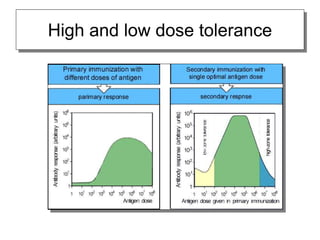
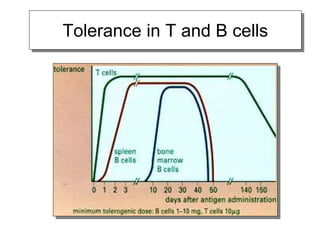
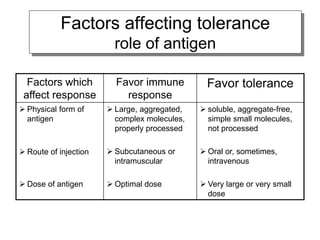
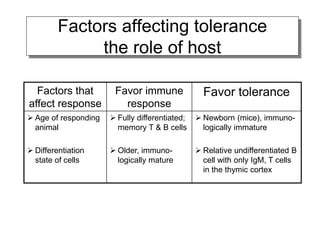
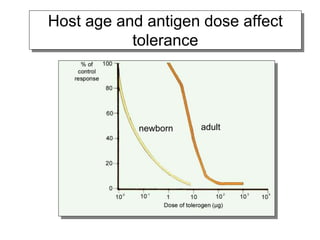
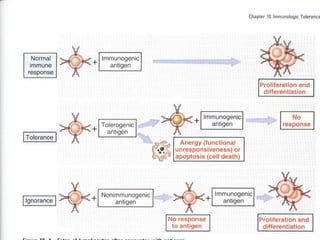
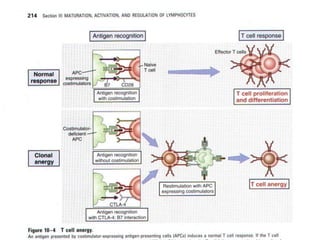
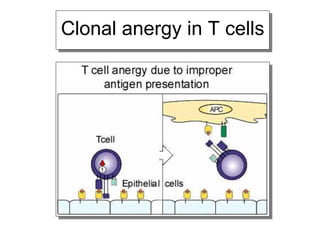
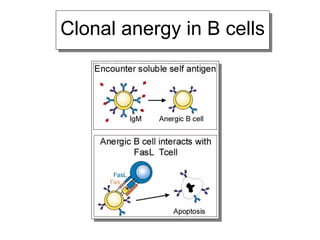
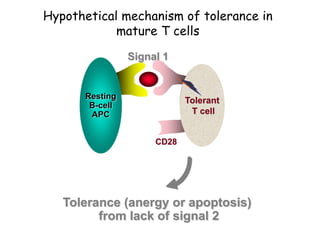
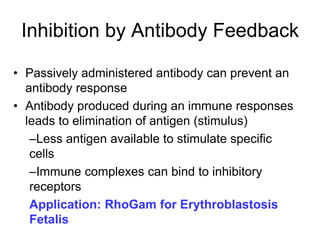
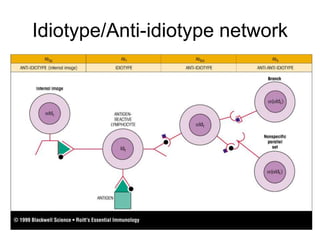
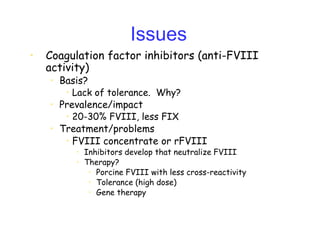
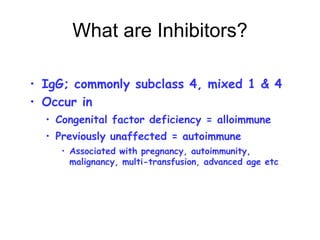
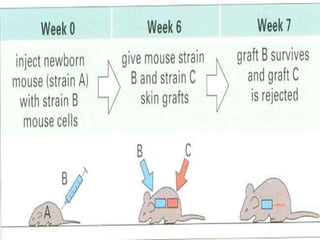
The document discusses immunologic tolerance, a specific unresponsiveness to antigens induced by exposure to those antigens. It details the mechanisms and types of tolerance (central and peripheral), the processes involved in self-tolerance, and potential applications in clinical medicine, including organ transplantation and treating autoimmune diseases. Key concepts include the induction of tolerance in lymphocytes, the role of tolerogens, and the distinctions between various forms of tolerance.
































![Types of Tolerance
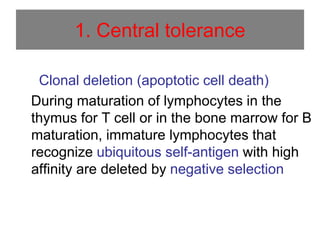
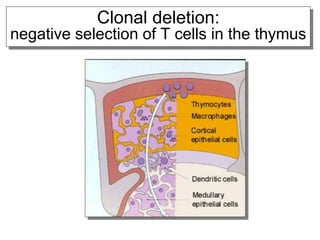
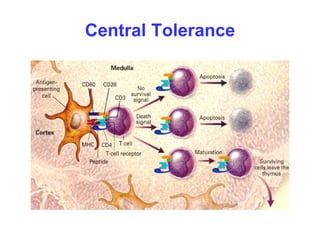
Central Tolerance :
It occurs during lymphocyte development.
[Thymus or Bone marrow]
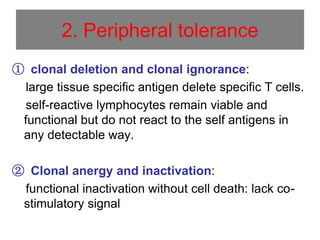
Peripheral Tolerance :
Occurs after lymphocytes leave the primary
organs.](https://image.slidesharecdn.com/immunological-tolerancedr-210417114717/85/Immunological-tolerance-dr-ihsan-alsaimary-78-320.jpg)