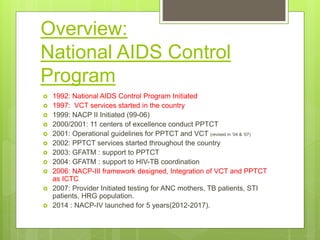
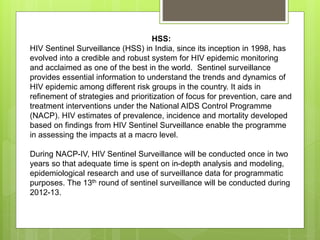
The document describes the evolution and components of India's National AIDS Control Program (NACP). It began in 1992 and is now in its fourth phase (NACP-IV) from 2012-2017. Key aspects include:
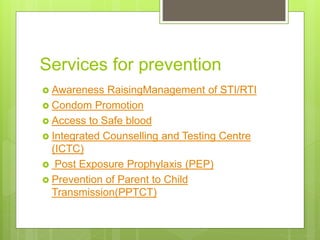
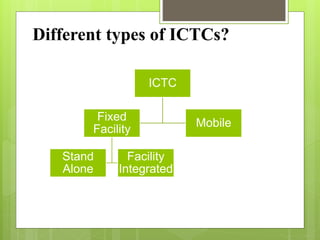
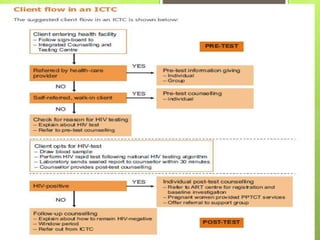
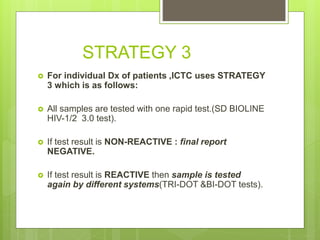
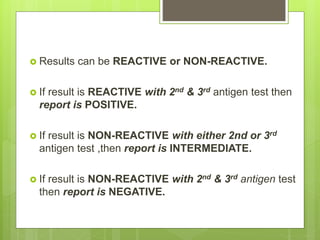
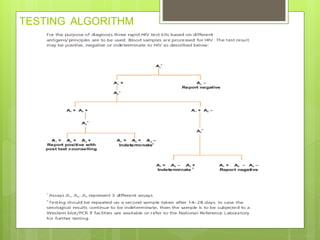
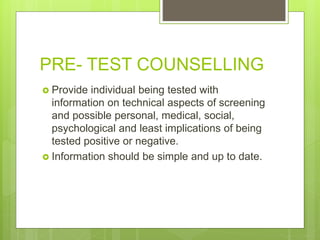
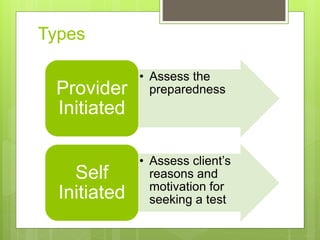
- Integrated Counselling and Testing Centers (ICTCs) were established in 2006 by integrating earlier Voluntary Counselling and Testing Centers (VCTCs) and Prevention of Parent-to-Child Transmission centers.
- NACP-IV has 5 components: prevention services, expanding information/education, comprehensive care/support/treatment, strengthening institutional capacities, and a strategic information management system.
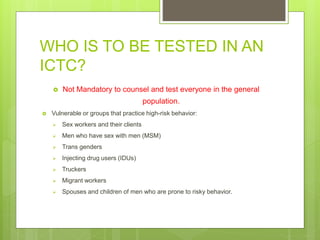
- Targeted interventions provide prevention, care, and treatment services focused on high-