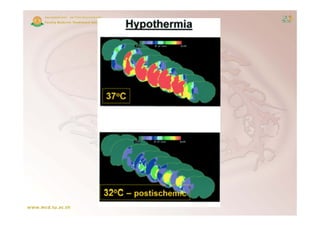
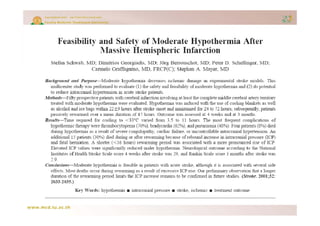
1) Therapeutic hypothermia after cardiac arrest and ischemic stroke has been shown to improve outcomes by reducing neurological injury through several mechanisms such as preventing blood-brain barrier disruption and reducing excitotoxic neurotransmitter release.
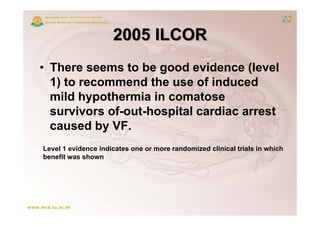
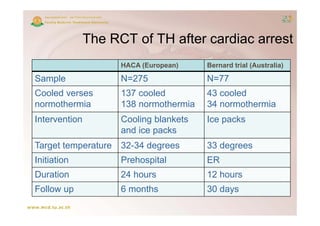
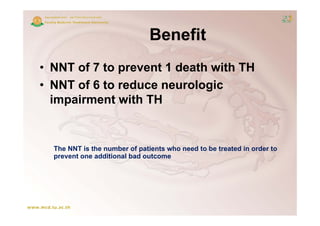
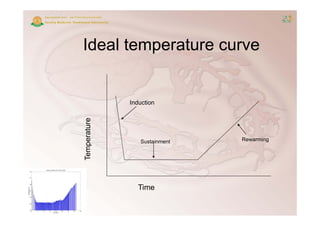
2) Two randomized controlled trials found that inducing mild hypothermia (32-34°C) for 24 hours in comatose cardiac arrest survivors improved survival and neurological outcomes with a number needed to treat of 6-7 to see benefit.
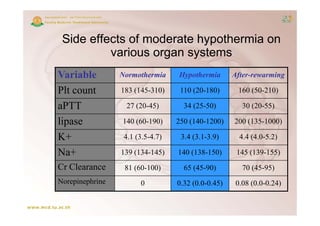
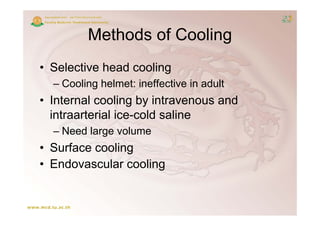
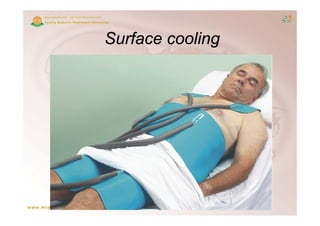
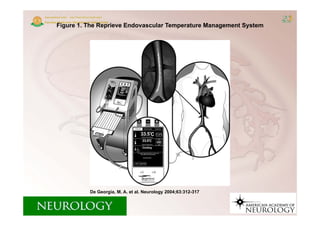
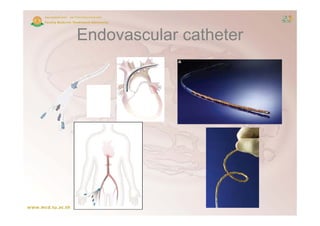
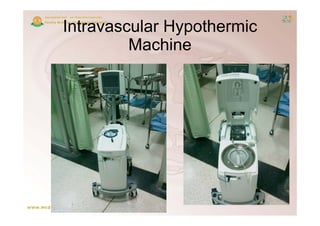
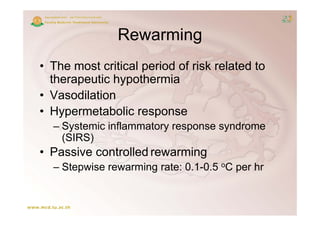
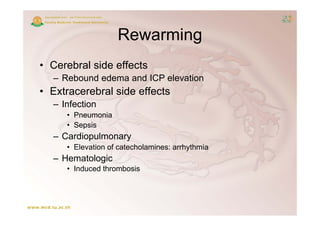
3) Methods to induce and maintain therapeutic hypothermia include surface cooling blankets, intravenous cold saline, endovascular cooling catheters, and cooling helmets. Careful rewarming is also important to avoid rebound injury.