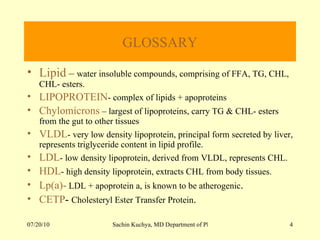
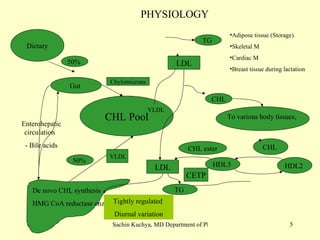
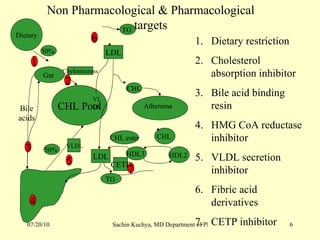
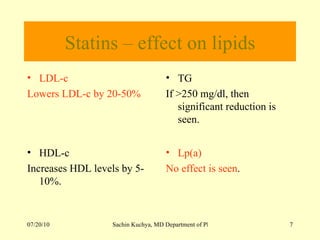
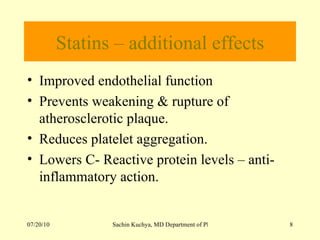
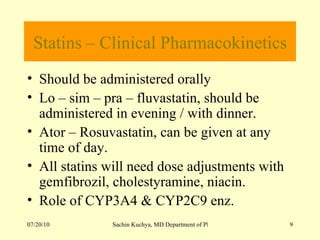
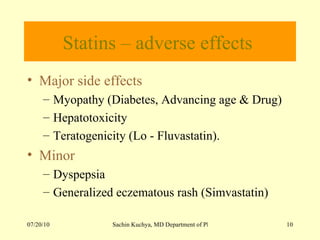
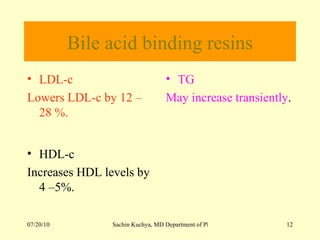
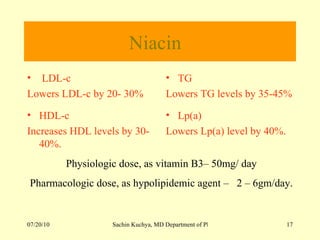
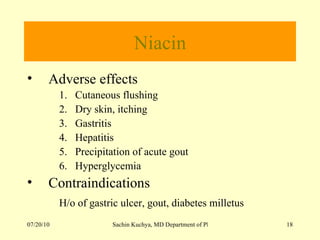
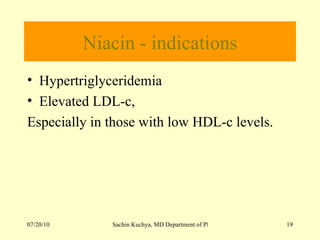
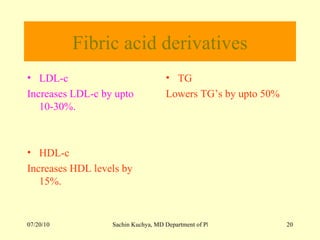
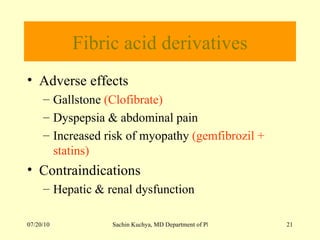
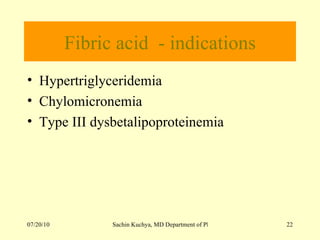
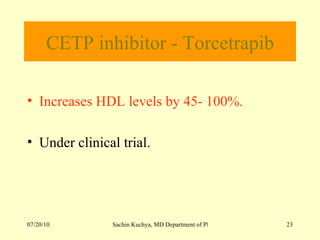
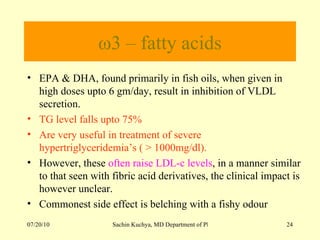
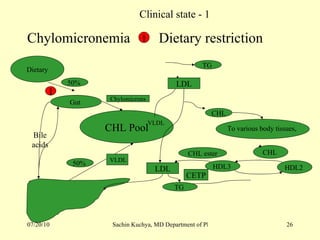
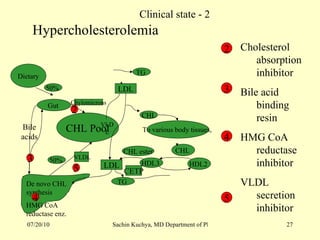
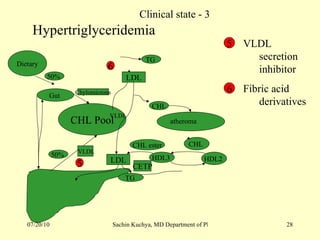
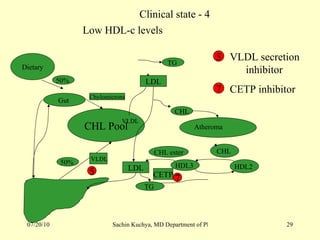
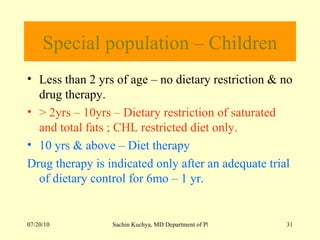
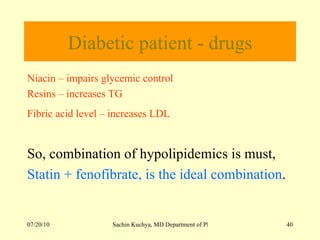
This document summarizes hypolipidemic agents used to treat various dyslipidemias and reduce cardiovascular risk. It discusses the physiology of lipid metabolism, pharmacological targets for lowering lipids, individual drug properties and combinations. Key drugs include statins, bile acid sequestrants, ezetimibe, niacin, fibrates and fish oils. The document also reviews use of these agents in special populations like children, women and diabetics.