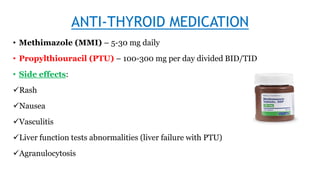
This document discusses the treatment of hyperthyroidism and thyroiditis. Treatment goals are to normalize TSH levels and correct clinical signs/symptoms. Initial treatment involves rest, sedation, and beta-blockers. Long term treatment uses antithyroid medications like methimazole or propylthiouracil to reduce thyroid hormone levels. Radioactive iodine or surgery may also be used. Nursing management focuses on providing a cool environment, minimizing stress, and monitoring for medication side effects like agranulocytosis.