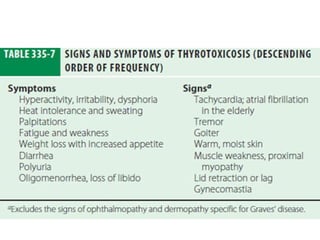
Thyrotoxicosis, primarily driven by hyperthyroidism, is characterized by hyperthyroid hormone levels and can manifest in conditions like Graves' disease, which accounts for a majority of cases. Key features include various clinical manifestations, including Graves' ophthalmopathy, and treatment options such as antithyroid drugs, radioactive iodine ablation, and surgery. Diagnosis requires careful hormonal evaluation, and the management approach varies based on the severity of symptoms and associated conditions.