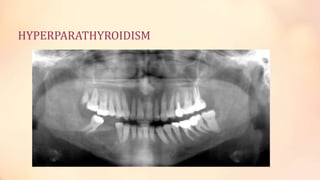
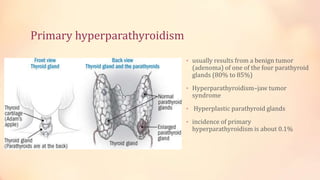
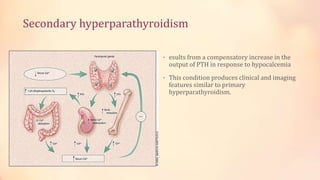
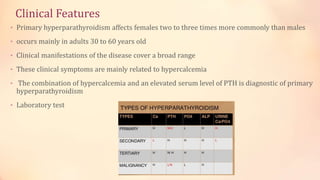
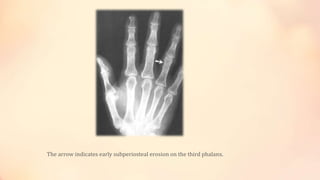
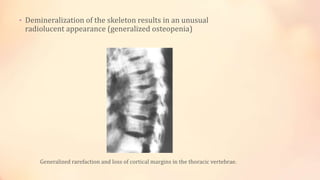
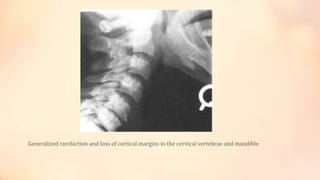
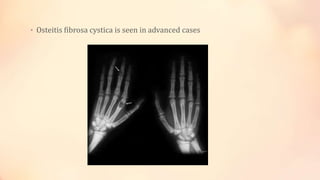
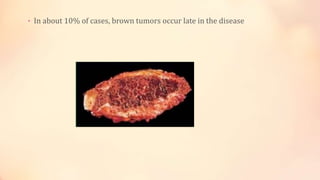
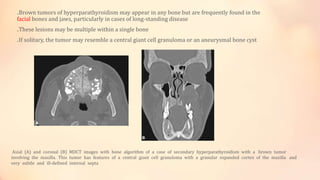
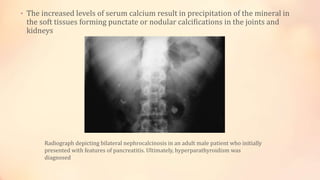
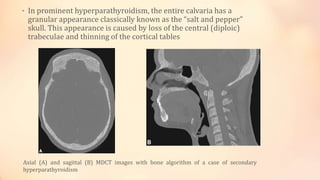
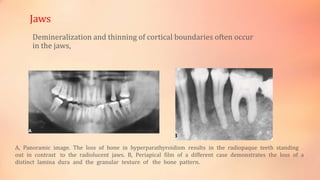
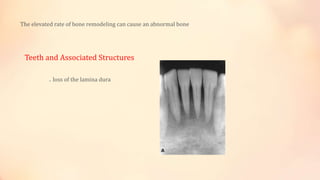
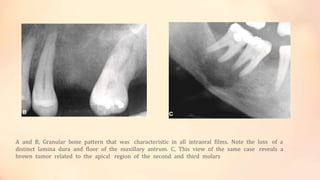
Hyperparathyroidism is a condition caused by excess parathyroid hormone that can lead to changes in bone structure and density. Primary hyperparathyroidism is usually caused by a benign tumor of the parathyroid glands and affects females more than males aged 30-60. Symptoms include those related to hypercalcemia like bone pain. Imaging may show features like brown tumors, osteopenia, and a "salt and pepper skull". Surgical removal of the tumor can resolve the condition and reverse changes except for sites of brown tumors.