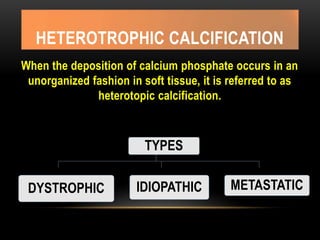
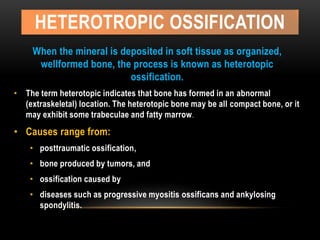
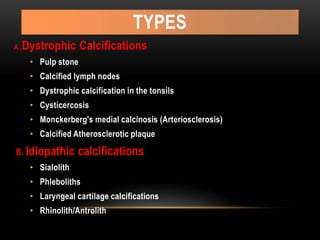
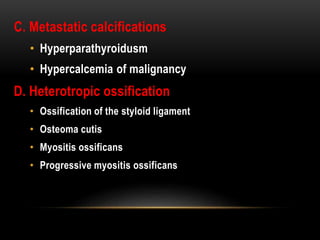
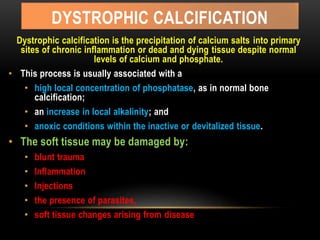
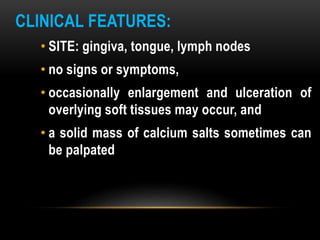
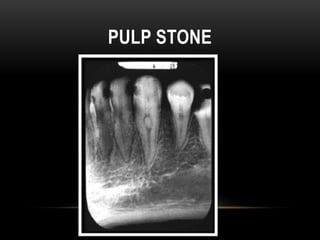
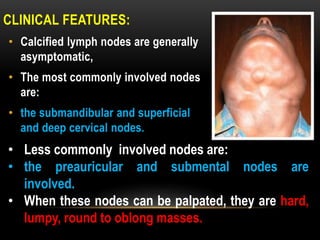
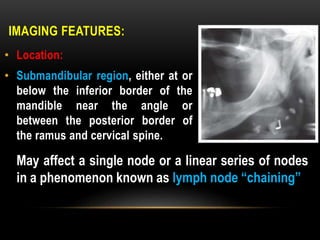
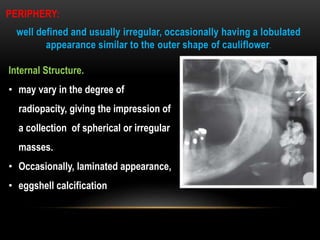
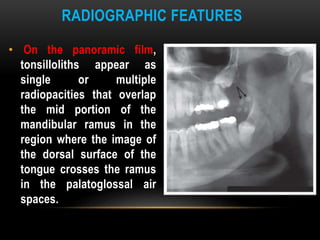
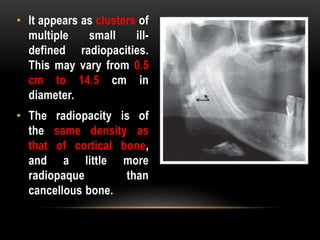
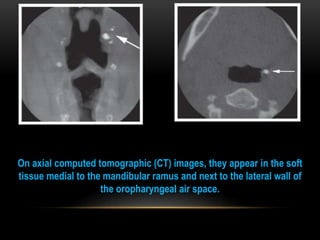
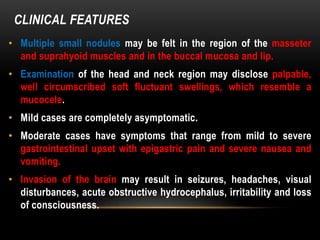
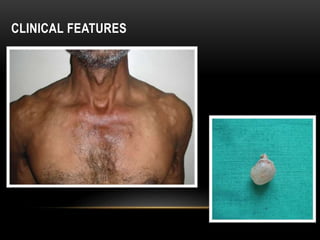
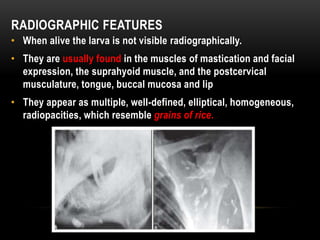
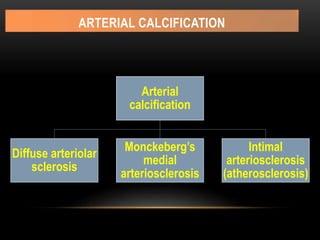
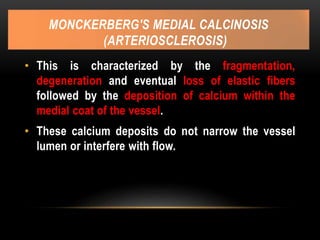
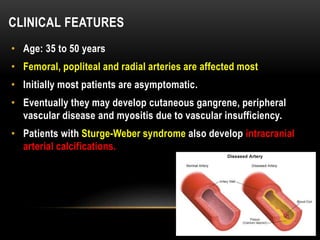
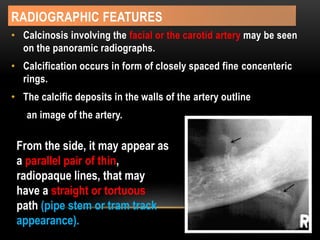
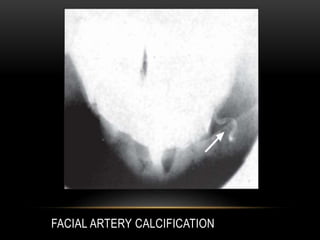
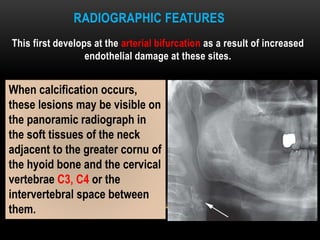
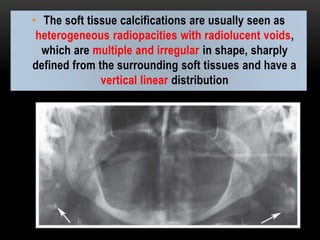
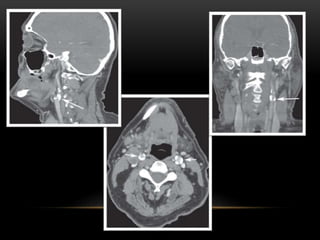
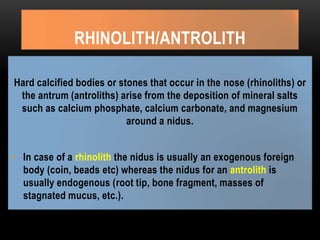
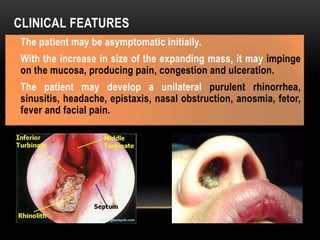
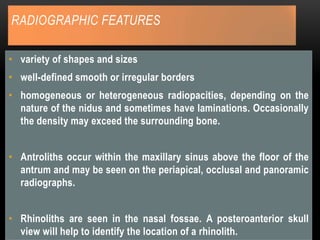
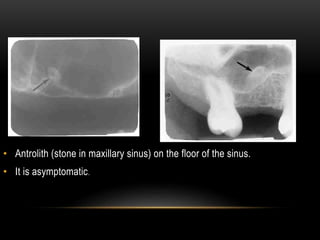
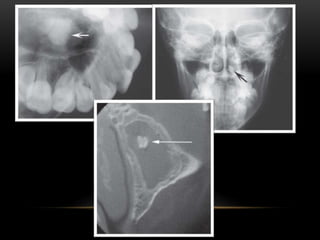
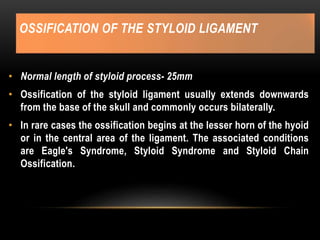
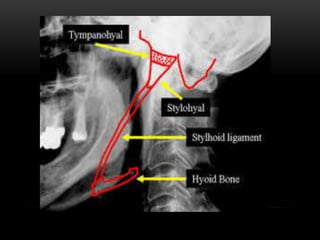
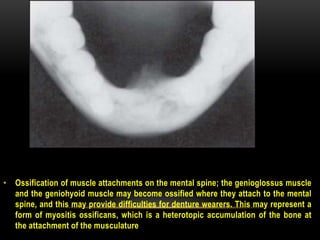
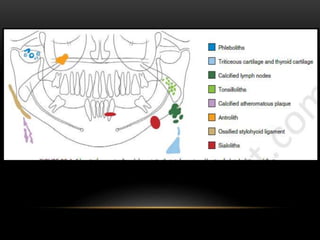
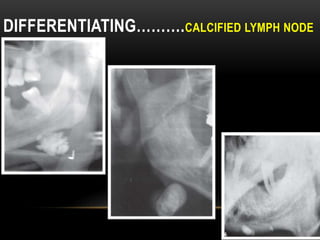
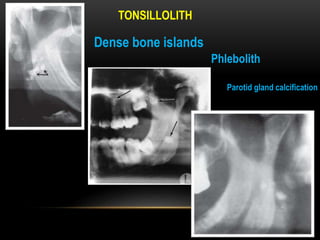
This document provides information about heterotrophic calcification and ossification. It discusses dystrophic, idiopathic, and metastatic types of calcification, as well as heterotopic ossification. Specific examples of dystrophic calcification are also described, including pulp stones, calcified lymph nodes, tonsilloliths, and cysticercosis. Monckeberg's medial calcinosis, an example of arterial calcification, is also summarized. Clinical features, imaging characteristics, and management are discussed for each condition.