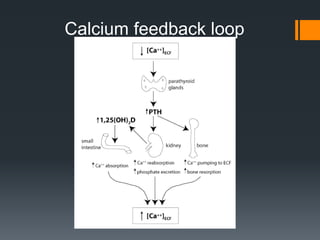
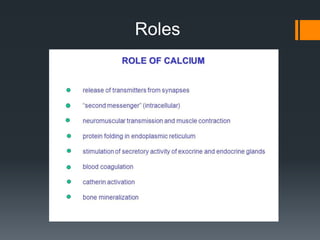
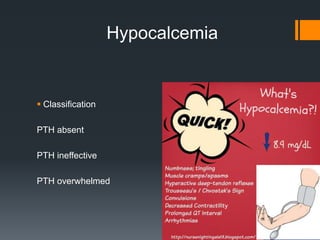
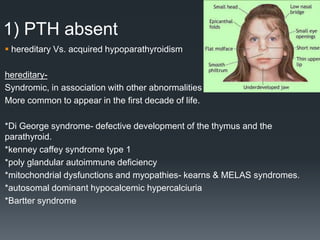
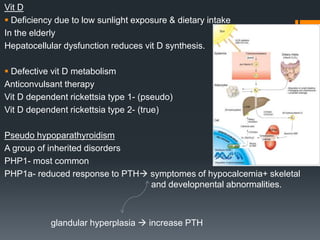
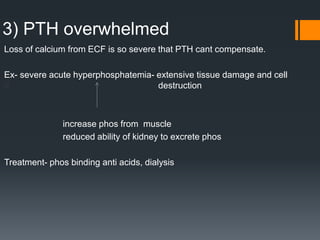
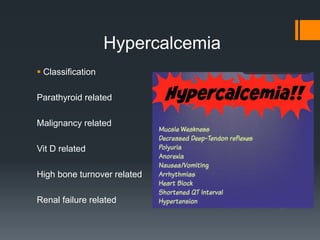
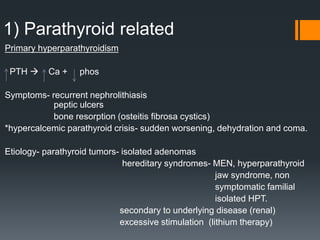
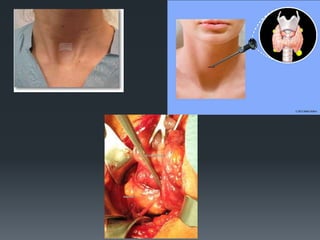
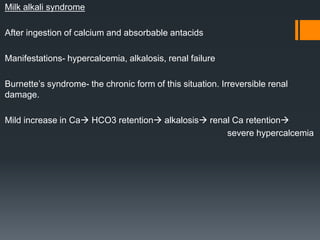
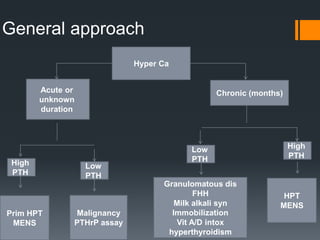
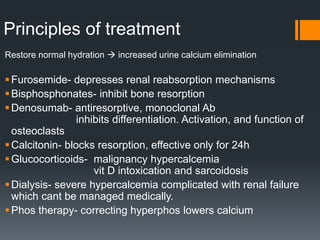
The document discusses the roles of hypocalcemia and hypercalcemia, focusing on classifications and causes such as parathyroid disorders, malignancies, and vitamin D-related issues. It details therapeutic approaches for managing these conditions, including medication, dietary modifications, and surgical interventions. Key points include the impact of hypoparathyroidism, chronic kidney disease, and hyperparathyroidism, among others, on calcium homeostasis.