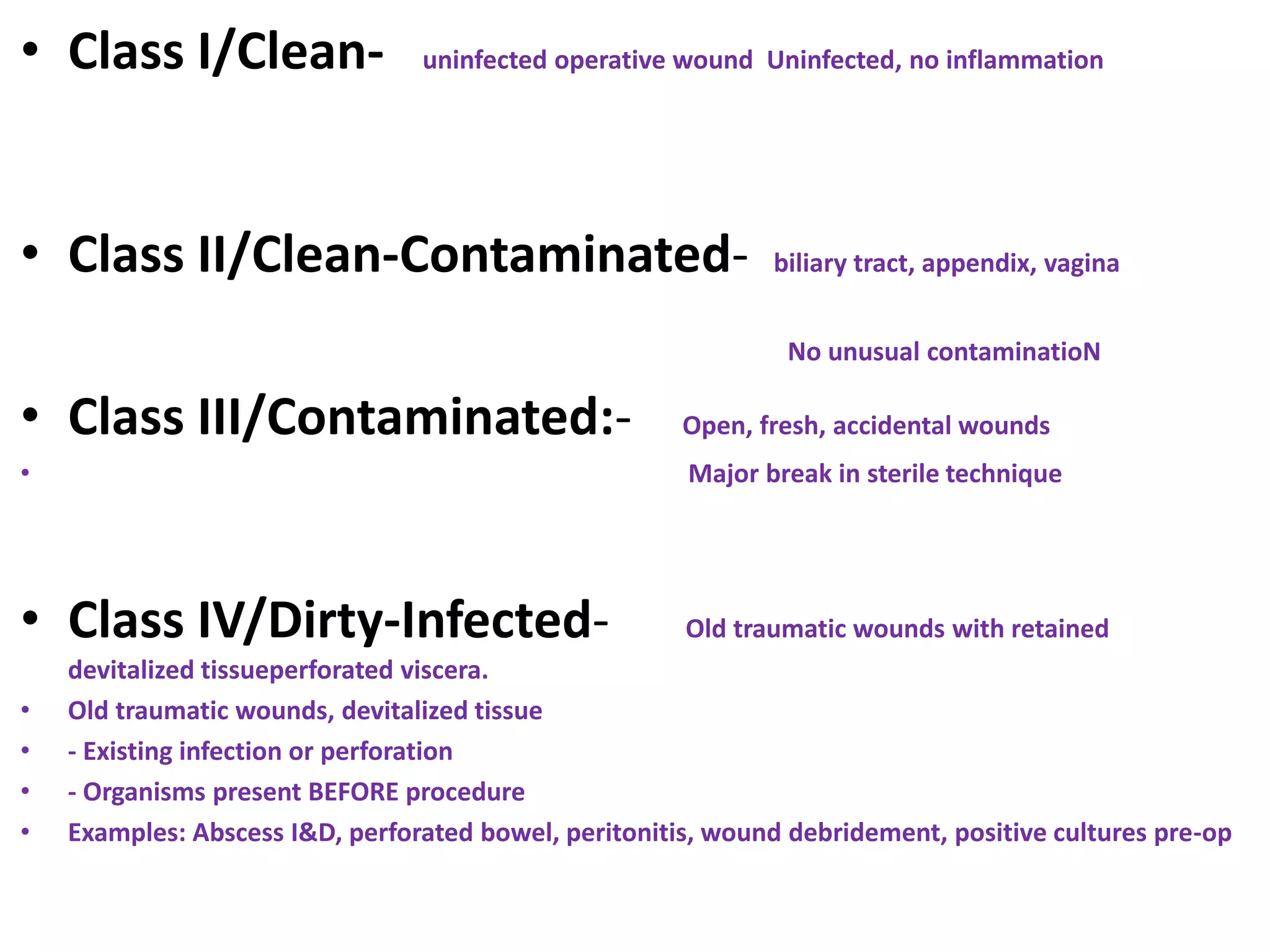
The document outlines healthcare-associated infections (HCAIs), particularly those occurring in hospitals, and details various types including ventilator-associated pneumonia (VAP), central line-associated bloodstream infections (CLABSI), and catheter-associated urinary tract infections (CAUTI). It emphasizes the importance of adherence to hygiene and infection control measures such as hand hygiene, personal protective equipment (PPE), and critical care bundles to prevent these infections. Moreover, it discusses prevention strategies, risk factors, and classification of surgical site infections (SSI), providing guidelines for best practices in healthcare settings.