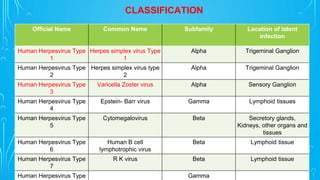
This document discusses herpes keratitis, caused by herpes simplex virus (HSV) or varicella zoster virus (VZV). It describes the clinical features of HSV keratitis, including infectious epithelial keratitis, neurotrophic keratopathy, stromal keratitis, and endothelitis. Treatment involves antiviral medications like acyclovir administered topically or orally, along with corticosteroids in some cases of stromal keratitis. Prophylaxis with oral antivirals can help reduce recurrences. Surgical treatment with corneal transplantation may be needed in cases of severe scarring or perforation.