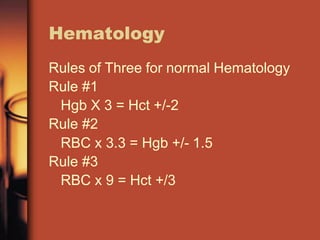
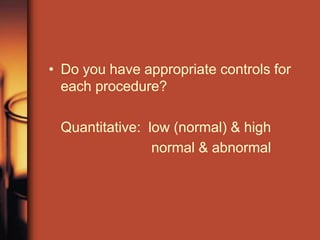
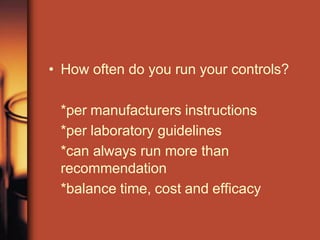
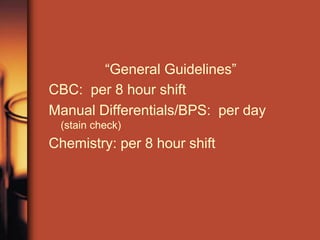
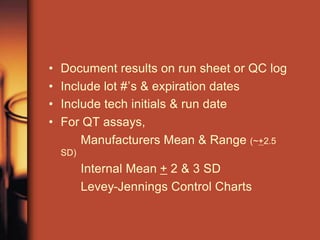
The document provides helpful hints and guidelines for hematology, chemistry, and coagulation testing. It discusses rules for validating complete blood count results, the need to calibrate instruments every 6 months or as needed, and tips for resolving low platelet counts or platelet clumping issues. The document also addresses quality control procedures like running controls according to specifications, establishing control ranges, using Levey-Jennings charts to monitor for patterns or shifts, and the importance of documentation and supervisor review for any control failures. It emphasizes treating controls like patient samples and verifying control results before releasing patient results.