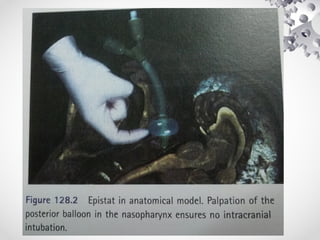
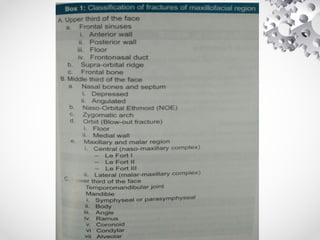
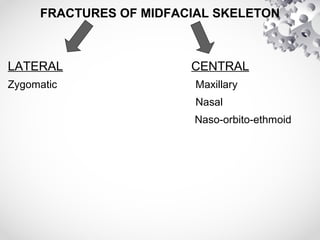
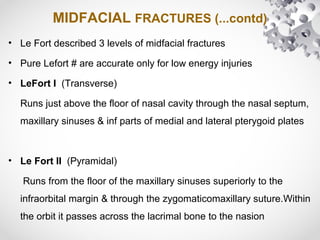
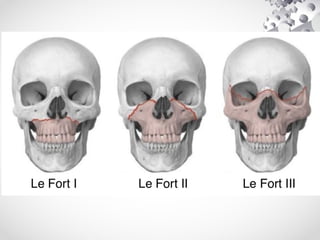
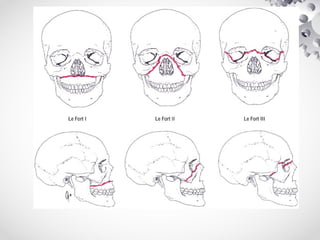
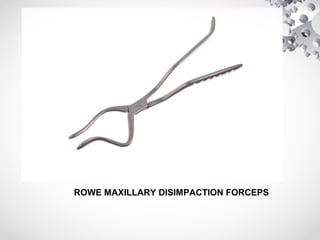
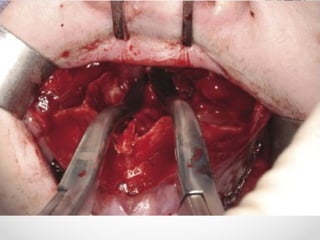
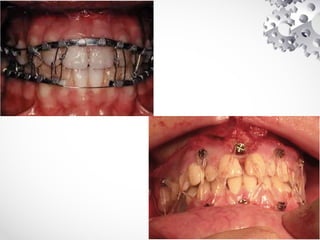
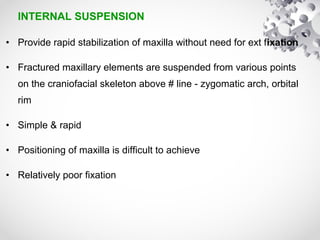
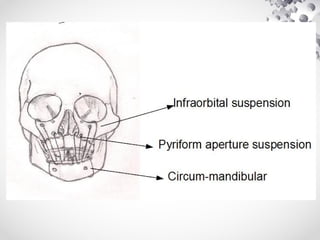
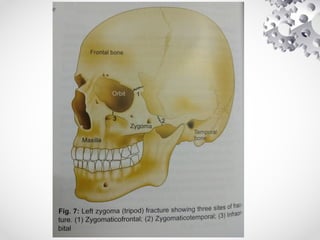
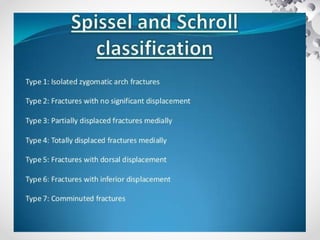
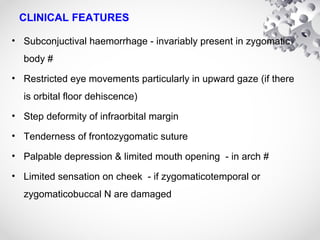
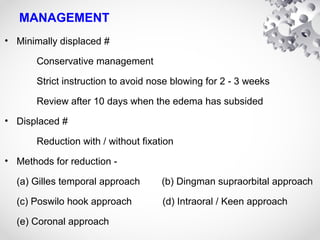
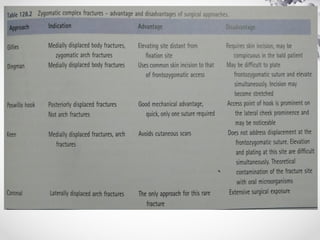
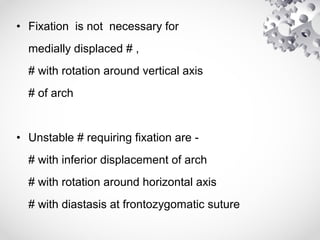
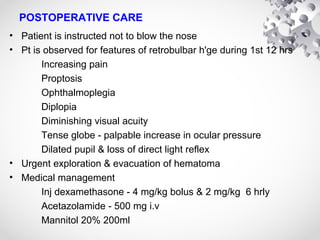
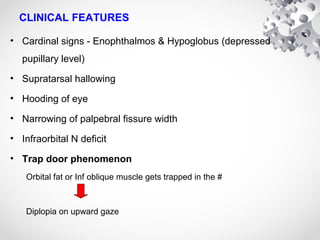
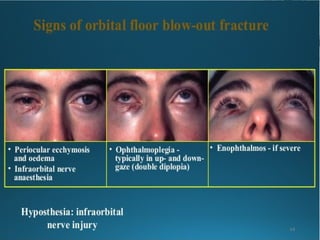
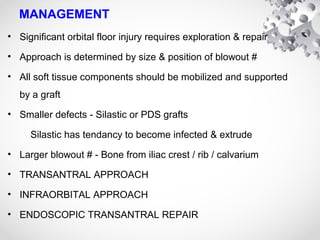
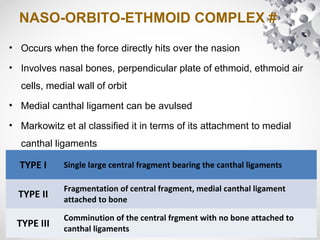
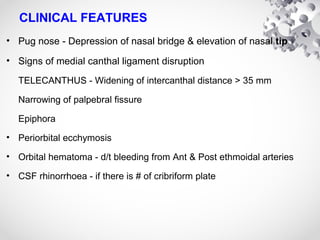
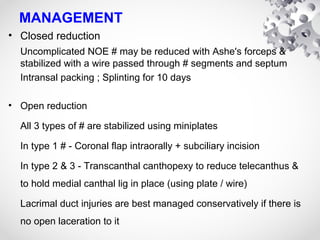
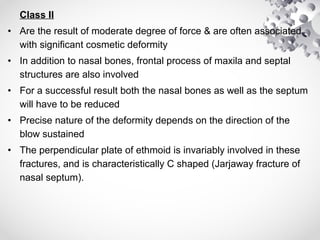
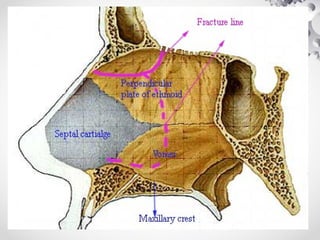
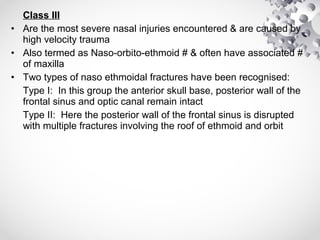
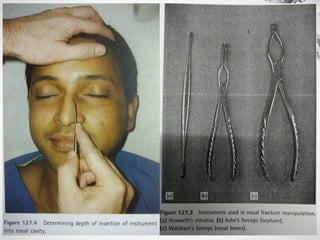
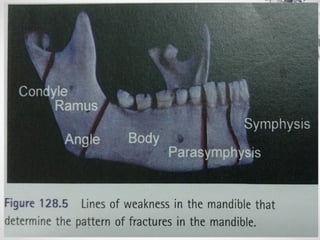
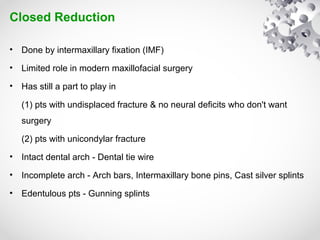
This document provides an overview of maxillofacial trauma. It discusses the classification, clinical features, and management of various types of midfacial fractures including Lefort fractures, zygomatic complex fractures, maxillary fractures, orbital floor fractures, and nasal bone fractures. For midfacial fractures, the document describes Lefort's classification system and approaches to reduction and fixation. It also outlines the primary and secondary surveys for maxillofacial trauma patients.