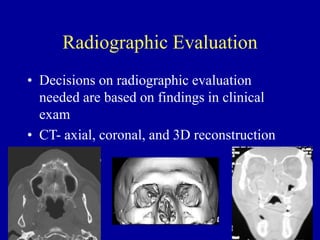
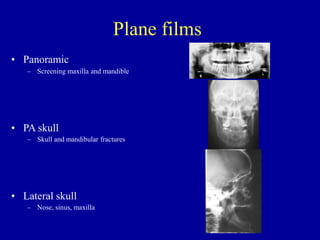
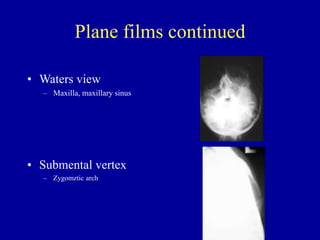
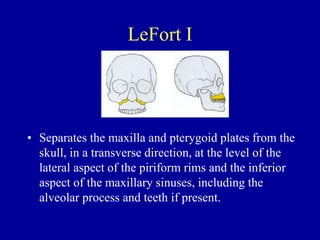
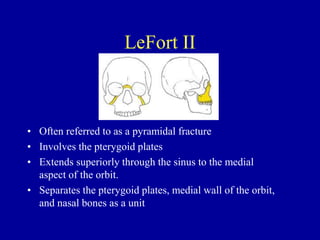
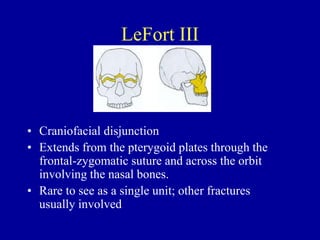
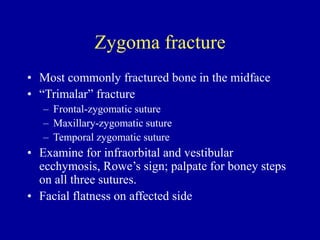
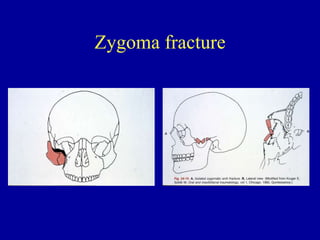
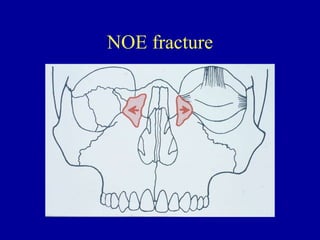
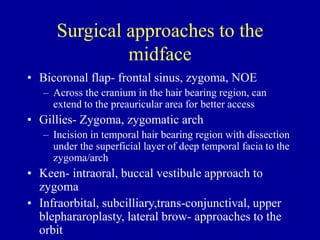
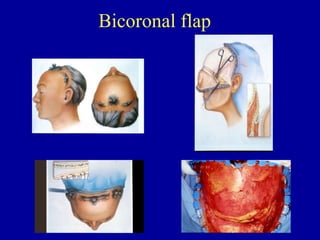
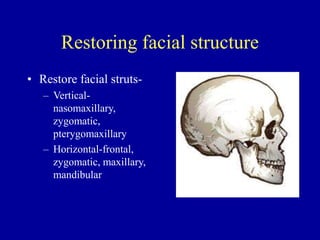
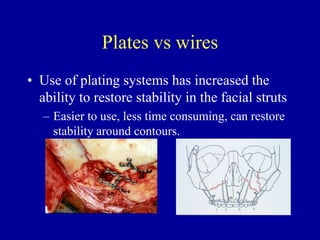
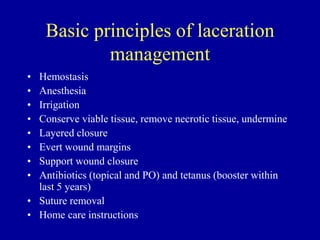
This document provides an overview of major midface trauma for medical professionals. It discusses evaluating and treating common midface fractures like Lefort fractures, zygomatic fractures, frontal sinus fractures, and naso-orbital-ethmoid fractures. Key points covered include performing a thorough trauma exam, using radiography like CT scans to identify fractures, classifying fracture types, understanding surgical approaches, and repairing facial structures and lacerations. The goals of treatment are to stabilize acute issues, prevent complications, restore function, and restore facial esthetics.