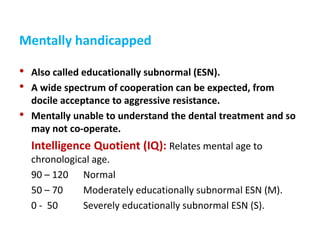
This document defines and classifies different types of handicapped children, including those who are physically, mentally, medically, emotionally, or socially handicapped. It discusses the importance of prevention for these children through dietary advice, oral hygiene instruction, fluoride treatment, fissure sealants, and regular checkups. It also emphasizes the need to carefully assess each child's medical history and abilities, consult their physician, and create a treatment plan tailored to the child and family's specific needs and capabilities. Behavioral management may require various techniques depending on the child's cooperation level, from mild sedation to general anesthesia in some cases.