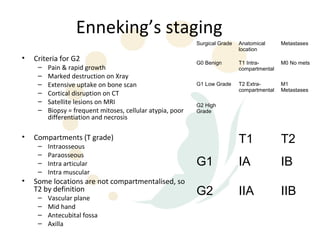
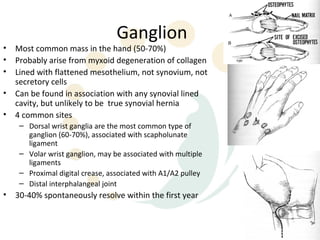
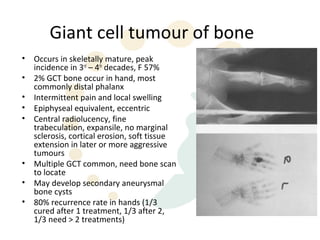
The document discusses common hand tumours such as ganglion, giant cell tumour of tendon sheath, and epidermoid inclusion cysts. It provides details on clinical presentation, investigations, classification systems, and treatment approaches for various bone and soft tissue tumours that can occur in the hand. Common malignant tumours of the hand discussed include synovial sarcoma, clear cell sarcoma, chondrosarcoma, and osteosarcoma.