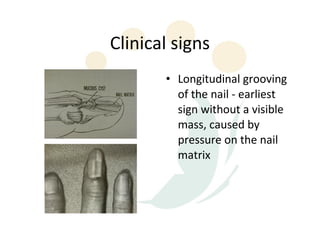
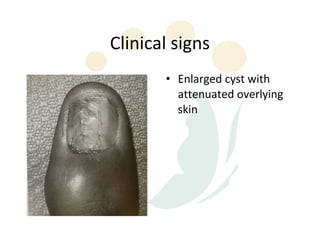
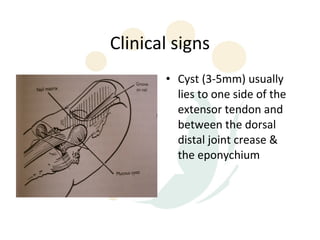
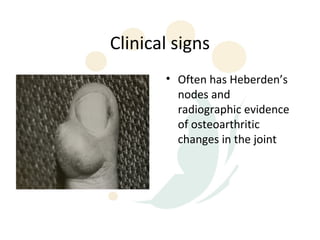
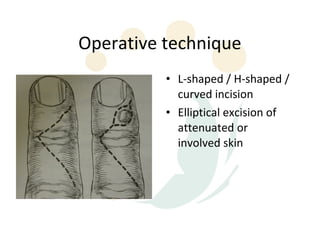
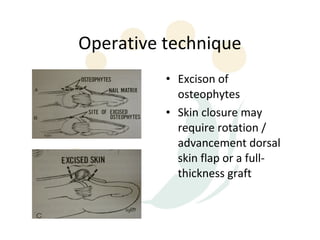
Mucous cysts of the DIPJ usually occur in older adults and are associated with osteoarthritis. They contain mucin and form from degeneration of joint structures. Clinically, they appear as nodules near the DIPJ that can cause nail deformities. Treatment involves surgical excision, sometimes with additional procedures like osteophyte removal. Complications include residual deformities, stiffness, skin issues, and recurrence due to incomplete excision or persistent arthritis.