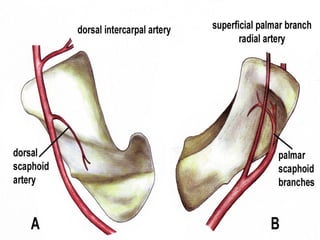
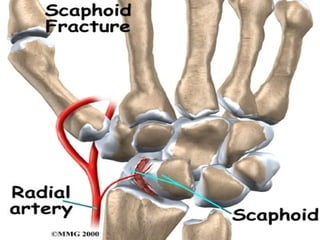
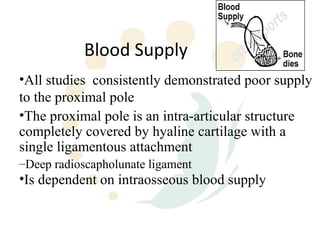
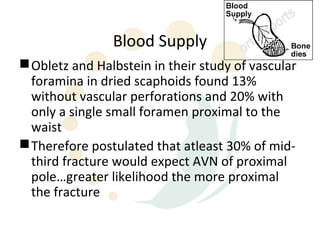
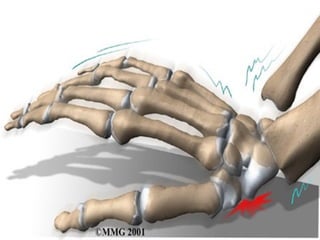
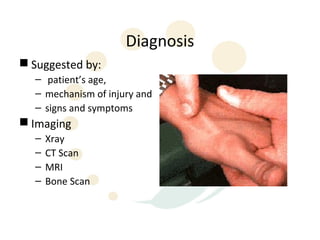
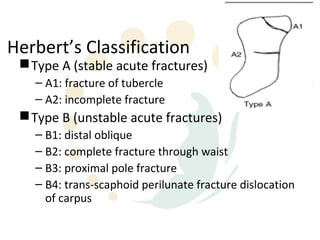
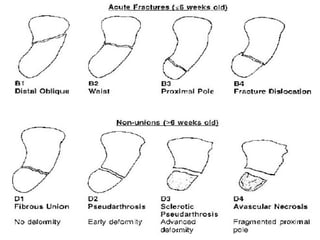
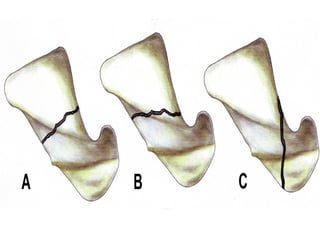
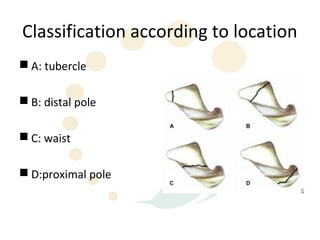
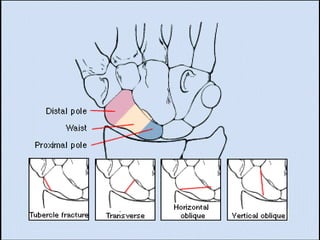
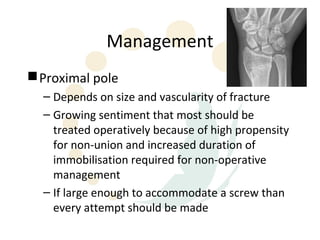
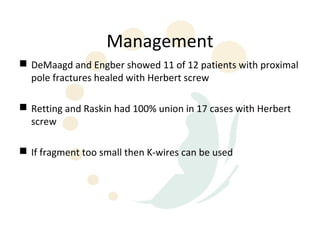
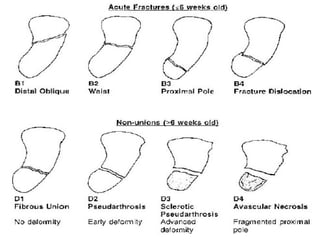
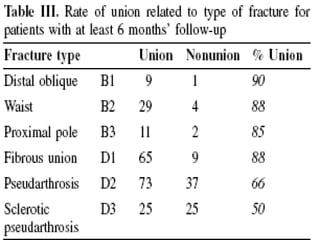
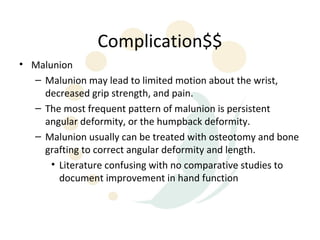
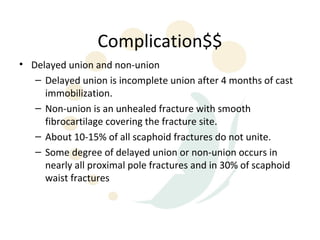
Scaphoid fractures are the most common carpal bone fractures, often occurring in young adults from falls on an outstretched hand. The scaphoid has a tenuous blood supply and is prone to non-union, especially for proximal pole fractures. Treatment depends on fracture type and stability, ranging from casting to operative fixation with screws. Complications include malunion, delayed union, non-union and avascular necrosis, requiring further procedures like bone grafting or carpal fusion.