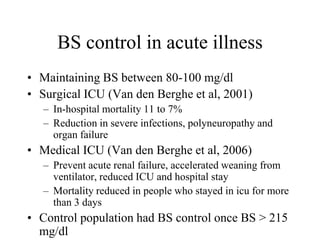
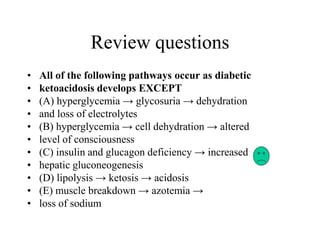
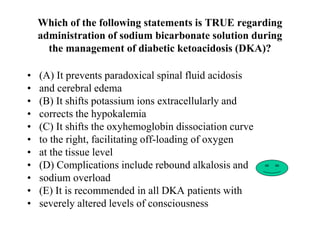
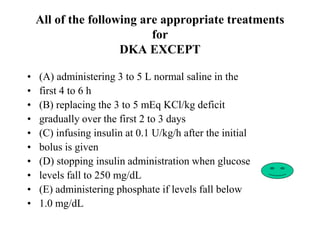
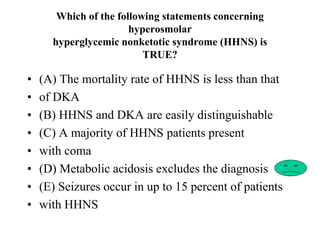
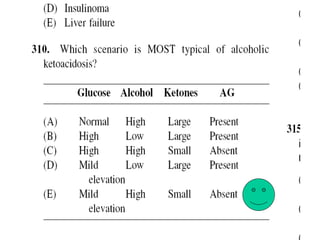
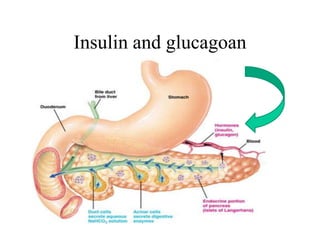
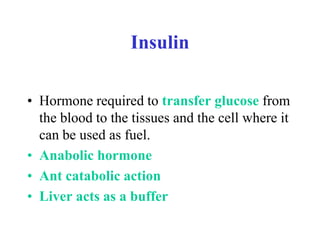
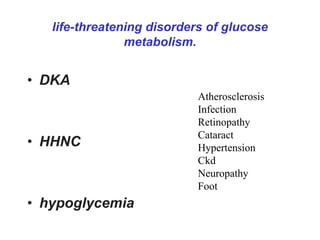
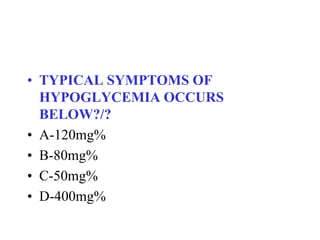
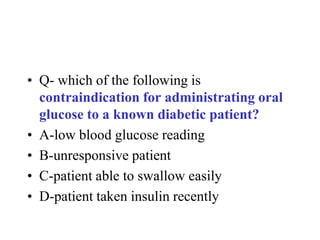
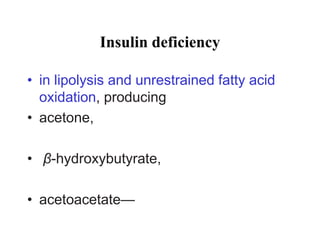
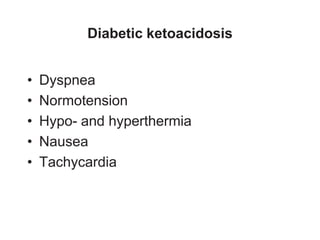
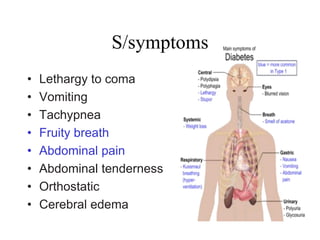
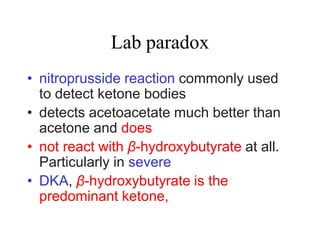
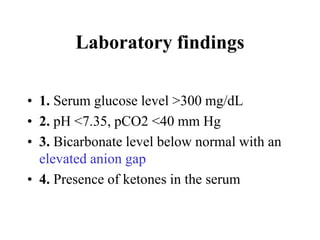
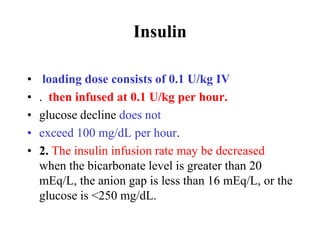
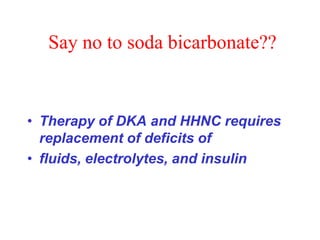
This document discusses glucose homeostasis and diabetic emergencies from an emergency perspective. It provides guidance on assessing altered mental status, including checking a blood sugar level. It describes insulin and its role in glucose metabolism. Diabetic ketoacidosis and hyperglycemic hyperosmolar state are life-threatening disorders that can result from lack of insulin or inability to use insulin properly. Proper treatment involves fluid resuscitation and insulin therapy while closely monitoring electrolytes. Hypoglycemia is also covered, noting it can result if insulin levels are too high.
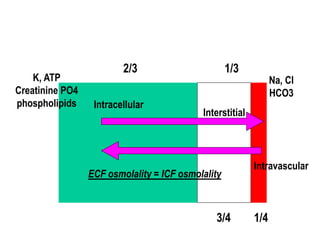
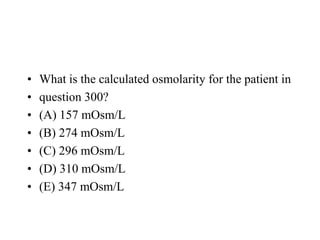
![Freezing point depression method
• Osmolarity (mOsm/L) = 2 × [sodium]
• + [glucose]/18 + [BUN]/2.8 +
[ethanol]/4.6](https://image.slidesharecdn.com/glucosehomeostasis-130509043243-phpapp02/85/Glucose-homeostasis-40-320.jpg)