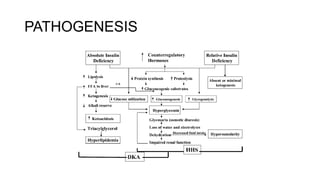
The document discusses the acute metabolic complications of diabetes mellitus, diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS). It describes the pathogenesis, clinical presentation, diagnostic evaluation and treatment of DKA and HHS. The treatment involves fluid resuscitation, insulin therapy to lower blood glucose levels, potassium supplementation and bicarbonate therapy is not recommended for DKA. Infection is a common precipitating factor for these conditions.