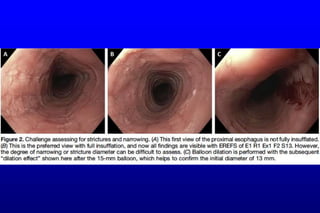
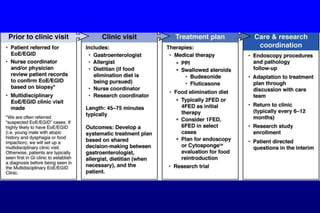
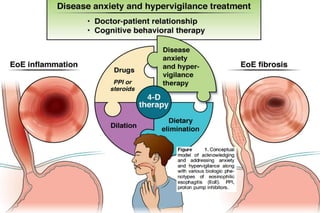
This document discusses best practices for endoscopically evaluating eosinophilic esophagitis (EoE). It recommends using the Eosinophilic Esophagitis Endoscopic Reference Score (EREFS) to systematically assess and record endoscopic features of EoE, including edema, rings, exudates, furrows, and strictures. A thorough examination is important to optimize diagnosis, assess treatment response, and monitor outcomes over time. Key steps include fully inflating the esophagus, carefully examining for subtle signs of narrowing or strictures, and obtaining multiple targeted biopsies from different locations to increase diagnostic yield.