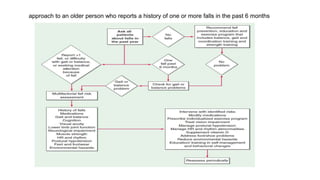
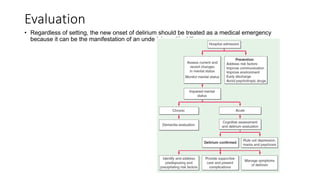
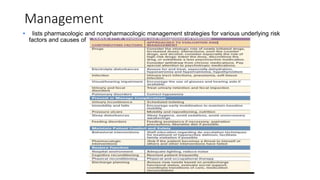
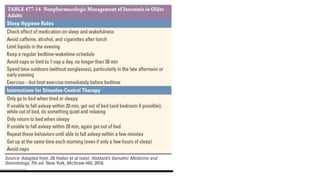
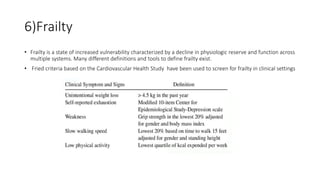
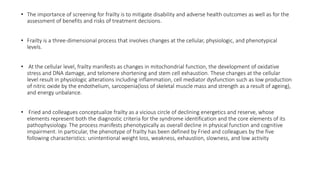
The document discusses geriatric syndromes, emphasizing the importance of prevention of disabilities as people age. It outlines common syndromes such as falls, polypharmacy, cognitive impairments, and urinary incontinence, detailing their causes, evaluation methods, and management strategies. Key interventions include regular screenings, medication reconciliation, and tailored treatment plans to address multifactorial health issues in older adults.