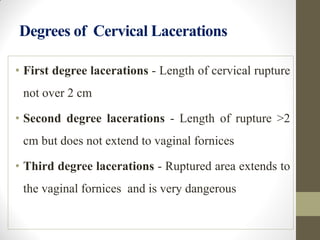
The document discusses injuries to the maternal birth canal during childbirth, highlighting their anatomy, classification, causes, diagnosis, and management. It emphasizes the importance of prevention, early detection, and effective management to minimize maternal morbidity, particularly concerning perineal, vaginal, and cervical injuries. Key factors affecting injury incidence include labor complications and the methods used during delivery, with detailed approaches for treatment and repair provided.